High upstage rate among nonmalignant papillary breast lesions diagnosed by image-guided core needle biopsy
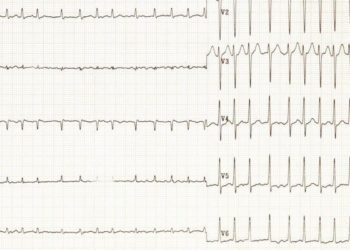
Image: CC
Key study points:
Primer: Image-guided core needle biopsy (CNB) has traditionally been used to help clinicians distinguish between benign papillary breast lesions and papillary carcinomas, their rare but malignant counterparts. CNB has high specificity (91-97%) for diagnosing malignant papillary lesions, but relatively poor sensitivity (74-89%), missing over one-quarter of papillary lesions that are ultimately found to be malignant (i.e. upstaged). Thus, while lesions that demonstrate signs of malignancy on CNB should be surgically excised, the dilemma of whether a “benign” papillary lesions should be surgically excised or clinically observed remains. Indeed, recent studies have found upstaging rates ranging from near zero to as high as 38% of benign papillary regions, thus suggesting that guidelines for excision may need to be specified for the individual institution level. To better define the upstage rate for benign papillary lesions obtained at CNB at Washington University and define clinical, imaging, and pathologic features associated with upstaging, the authors conducted this retrospective case review.
Background Reading:
- Accuracy of core needle biopsy diagnosis in assessing papillary breast lesions: histologic predictors of malignancy [Nature]
- Papillary Lesions of the Breast With and Without Atypical Ductal Hyperplasia Can We Accurately Predict Benign Behavior From Core Needle Biopsy? [American Journal of Clinical Pathology]
- Role of Mammography, Ultrasound and Large Core Biopsy in the Diagnostic Evaluation of Papillary Breast Lesions [Oncology]
This [retrospective case review]: 128 patients with nonmalignant papillary breast lesions diagnosed with image-guided CNB were studied. Of these, 14 were subsequently found to have malignancy after surgical incision, thus indicating an upstage rate of 11%. Patients who had upstaged lesions were more likely to be older (median age of 65 versus 56 in those whose lesions were benign, p=0.04). Further, masses were more likely to be upstaged compared to nonmass lesions (p=0.03), though most masses (77%) were found to be benign. Patients were upstaged lesions were more likely to have less tissue obtained and more likely to have commentary on their pathology reports (p<0.01) suggesting that the pathologist felt some uncertainty regarding the benign diagnoses of these lesions.
In sum: This study demonstrated a high rate of upstaging (11%) among benign papillary lesions diagnosed by CNB at Washington University, with upstaging associated with age of the patient, with the presence of mass on imaging, the lack of tissue obtained on biopsy, and decreased confidence on the part of the pathologist in diagnosing the lesion as benign. This study is one of the largest published patient series addressing the clinical question of upstaging in benign papillary lesions. Further, it is the first to suggest that the confidence of the pathologist may be predictive of upstaging. Thus, the authors argue that though their high rate of upstaging suggests that “surgical excision is the most prudent action when a papillary lesion is diagnosed at CNB,” the views of the pathologist regarding the diagnosis may play a key role in how these lesions should ultimately be handled. First, if a papillary lesion is suspected, efforts should be made to obtain more tissue at CNB to aid the pathologist in diagnosis. Second, if a pathologist has any reservations regarding the benign nature of a papillary lesion, surgical excision would be the best course of action. However, if the clinical, imaging, and pathologic features all suggest a benign diagnosis, then clinical observation may be a possible alternative.
Limitations faced by their study include: 1) Given the wide variability among the practice of different pathologists and requirements at differing institutions, the presence of commentary may not be applicable as an indication of pathologist confidence in other clinical settings and 2) The patient population was not randomized to surgical excision versus clinical observation, thus any conclusions regarding these two groups may be affected by confounders.
Click to read the study in Radiology
By MK
© 2012 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. DISCALIMER: Posts are not medical advice and are not intended as such. Please see a healthcare professional if you seek medical advice.