2 Minute Medicine Rewind April 30, 2018
Azithromycin to Reduce Childhood Mortality in Sub-Saharan Africa
Oral azithromycin is the mainstay of treatment for trachoma, and has been distributed throughout sub-Saharan Africa in an effort to eliminate strains of chlamydia that cause the disease. Recent studies have suggested that mass distribution of azithromycin may reduce childhood mortality, although a consensus has not been reached in the field. In this cluster-randomized controlled trial, 190,238 children age 1 to 59 months from 1,512 communities in Malawi, Niger, and Tanzania were randomized to receive either two doses of oral azithromycin or placebo per year to determine the impact on aggregate all-cause mortality. At the end of the five 6-month census periods, researchers found that the annual mortality rate of the azithromycin group (14.6 deaths per 1000 person-years) was lower than that of the placebo group (16.5 deaths per 1000 person-years). Overall, community-level, intention-to-treat analysis showed that mortality was 13.5% lower in the azithromycin group than in the placebo group (95% CI 6.7% to 19.8%, p<0.001). The effect of azithromycin on observed mortality was greatest in children 1 to 5 months of age (24.9% lower than placebo, 95% CI 10.6% to 37.0%, p=0.001) and in the Niger subgroup (18.1% lower than placebo, 95% CI 10.0% to 25.5%, p<0.001). Mortality rates were not significantly different in the Malawi or Tanzania subgroups. Investigation is currently under way to identify the mechanism by which azithromycin reduced mortality in this trial. Overall, results suggest that oral azithromycin can reduce childhood mortality in sub-Saharan Africa. Limitations of this study include the lack of detailed information on individual children and communities and potential lack of generalizability to other geographic areas. Long-term follow up will be necessary in monitoring for antibiotic resistance and related sequelae.
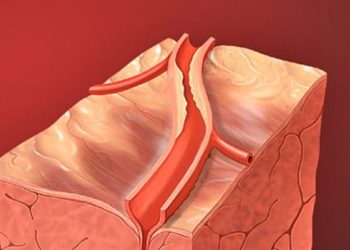
Tenecteplase versus Alteplase before Thrombectomy for Ischemic Stroke
Acute ischemic stroke is typically treated with intravenous thrombolysis via alteplase infusion followed by endovascular thrombectomy. Tenecteplase, a genetically modified variant of alteplase, has greater fibrin specificity, is less expensive, and can be administered as a bolus instead of an infusion. However, whether tenecteplase produces better clinical and functional outcomes than alteplase is still unclear. In this randomized controlled trial, 202 patients with ischemic stroke and occlusion of the internal carotid, basilar, or middle cerebral arteries eligible for endovascular thrombectomy were randomized to receive tenecteplase or alteplase within 4.5 hours of symptom onset to assess whether tenecteplase is non-inferior and superior to alteplase in reperfusion and thrombolysis. The primary outcome was reperfusion greater than 50% of the involved ischemic territory or an absence of retrievable thrombus in the target vessel at the time of initial angiographic assessment. Researchers found that reperfusion or absence of retrievable thrombus occurred in more patients who received tenecteplase (22%) compared to those who received alteplase (10%) (incidence difference 12%, 95% CI 2% to 21%, p=0.002 for noninferiority, OR 2.6, 95% CI 1.1 to 5.9, p=0.02 for superiority). Tenecteplase also resulted in improved 90-day functional outcome compared to alteplase based on the modified Rankin scale score, a measure of neurologic deficit (OR 1.7, 95% CI 1.0 to 2.8, p=0.04). This study was limited in that the results only apply to patients with large-vessel occlusions and patients eligible for thrombolysis, a population that represents approximately 13% of all patients with ischemic stroke. Overall, this study demonstrates that tenecteplase may be superior to alteplase in tissue reperfusion and overall functional outcome. Ongoing studies are investigating the noninferiority of tenecteplase in patients who are not eligible for endovascular thrombectomy.
Approximately one-third of patients with major depressive disorder (MDD) do not respond to pharmacotherapy or psychotherapy. Repetitive transcranial magnetic stimulation (rTMS), a form of non-invasive brain stimulation, is a well-established treatment option, but its adoption has been slow. Barriers to adoption may include high cost and the long duration of treatment sessions. Recent meta-analyses have suggested that intermittent theta burst stimulation (iTBS), a newer form of rTMS that boasts shorter treatment sessions, is superior to sham treatment. However, whether iTBS performs comparably to conventional rTMS in the treatment of MDD is unknown. In this randomized controlled trial, 414 patients with treatment-resistant MDD were randomized to receive 10 Hz rTMS or iTBS to determine whether iTBS is non-inferior to rTMS in the reduction of depressive symptoms and in rates of response and remission. Depressive symptoms were evaluated using HRSD-17 scores. Researchers found that reduction in HRSD-17 scores after treatment was similar in the two groups, with a reduction from 23.5 to 13.4 in the rTMS group and from 23.6 to 13.4 in the iTBS group (adjusted difference 0.01, p=0.0011 for noninferiority). Remission and response rates following iTBS were also non-inferior to those of rTMS, (p=0.0005 and 0.0005, respectively). The average pain score was lower in the rTMS group (3.4 SD 2.0) than in the iTBS group (3.8, SD 2.0) (p=0.011). There was no significant difference in the number of serious adverse events between groups (p=0.6232). This study therefore shows that in patients with treatment-resistant MDD, iTBS is non-inferior to 10 Hz rTMS for the treatment of MDD. A limitation of this study was the absence of a placebo condition to equalize session durations, thus treatment allocation was not blinded.
Periodic supervised treadmill exercise during medical center visits has been shown to improve walking performance in patients with lower-extremity peripheral artery disease (PAD). The impact of home-based treadmill exercise, however, has not been evaluated. In this randomized controlled trial, 200 patients with an ankle brachial index (ABI) of 0.90 or less at baseline or with laboratory or angiography-proven PAD were randomized to a home-based exercise intervention or usual care (no intervention) to determine whether home-based exercise improves 6-minute walk distance at 9 months. Researchers also tracked changes in Walking Impairment Questionnaire (WIQ) scores and pain interference as per the Patient-Reported Outcomes Measurement Information System (PROMIS) questionnaire. The home-based exercise intervention consisted of individualized telephone coaching and a wearable activity monitor. After 9 months of follow-up, researchers found that there was no significant difference in mean change in 6-minute walk distance between groups (between-group difference -8.9 meters, 95% CI -26.0 m to 8.2 m, p=0.31). In addition, there was no significant difference in change in the mean WIQ distance score in the exercise group (from 38.0 to 52.2, within-group difference 10.6) compared with the usual care group (from 37.7 to 46.1, within group difference 4.8) (between-group difference 5.8, 95% CI -3.0 to 14.7, p=0.20). Notably, the PROMIS pain interference score worsened in the exercise group (between-group difference 3.5, 95% CI 1.3 to 5.8, p=0.002). Overall, results from this study do not support a role for home-based exercise without periodic medical center visits in the improvement of walking performance in patients with PAD.
Last year, the American Academy of Pediatrics (AAP) and the American Heart Association (AHA) published new clinical practice guidelines for the diagnosis and management of elevated blood pressure (BP) in children. Chiefly, obese and overweight children were excluded from reference data, and new cutoffs were developed to better define elevated BP, stage 1, and stage 2 hypertension. The consequences of these new guidelines on the prevalence and severity of elevated BP among US children have not yet been established. In this case-control study, the new guidelines were applied to reclassify the BP of 15,647 healthy, low-risk children aged 5 to 18 years. Cases (children whose BP was reclassified upward) were compared to sex, age and height matched controls (normal BP) to identify clinical and laboratory risk factors for newly classified hypertension. Researchers found that the estimated (weighted) prevalence of elevated BP increased from 11.8% (95% CI 11.1% to 13.0%) using previous guidelines to 14.2% (95% CI 13.4% to 15.0%). Moreover, 5.8% of children were reclassified upward, and these children were more likely to be male, taller, and younger than normotensive children. After matching for sex, height, and age, cases were more likely to be overweight or obese (55.9%) compared to controls (35.0%) (p<0.001). In addition, cases were more likely to have elevated concentrations of lipids (22.6% of cases vs. 10.7% of controls had elevated triglycerides, p<0.001) and hemoglobin A1c (3.4% of cases vs. 0.6% of controls, p=0.02). Limitations of this study include insufficient numbers to perform race-, sex-, and age-specific subgroup analyses. Overall, this study suggests that reclassified children represent a high-risk population that may require close follow-up and possible treatment for elevated BP.
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.