2 Minute Medicine Rewind September 22, 2025
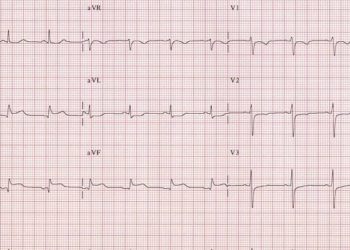
1. The lactate-to-albumin ratio was an independent predictor of 28-day mortality in hypertensive patients with atrial fibrillation.
Evidence Rating Level: 2 (Good)
Atrial fibrillation (AF) is the most common arrhythmia in critically ill patients. Patients with hypertension and AF present with greater clinical severity, which complicates prognosis. As traditional prognostic indicators may not fully capture the complexity of this condition, lactate-to-albumin ratio (LAR), a composite marker of metabolic stress and nutritional status, has been proposed to enhance prognostic precision. The role of LAR had been studied in general intensive care unit (ICU) populations, but not specifically in critically ill hypertensive patients with AF. This study investigated the association between LAR and mortality in hypertensive patients with AF. This retrospective cohort study used data from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database between 2008 and 2022 and included hypertensive patients >18 with AF and LAR values obtained within the first 24 h after ICU admission. Patients were divided into two groups based on 28-day in-hospital survival: a survivor group and a nonsurvivor group. The primary endpoint was mortality within 28 days of ICU admission. Out of the 1087 patients included in the study (mean [SD] age = 76.78 [11.35], 478 [43.97%] female), 839 survived while 248 did not, resulting in a 28-day mortality rate of 22.8%. Compared with survivors, nonsurvivors had higher LAR values (0.74 vs. 0.52, p < 0.001). Increase in LAR was independently associated with greater risk of 28-day mortality (adjusted HR 1.03, 95% CI 1.01–1.06). Additionally, LAR had superior predictive ability (area under the curve [AUC] 0.661) compared with other biomarkers. Participants with high LAR (> 0.605) had a higher risk of mortality compared to those with low LAR (< 0.605) (HR 2.55, 95% CI 1.97–3.30). Overall, this study found that LAR is an independent predictor of short-term mortality in critically ill hypertensive patients with AF, highlighting its potential for risk assessment and tailored care in this population. Future studies with larger sample sizes are needed to confirm these results.
Outcomes of Critically Ill Adult Patients With Acute Encephalitis
1. Poor prognosis (disability or death) at 3 months was observed in half of adult patients with severe encephalitis requiring intensive care unit care.
2. 1-year recovery trajectories varied by cause of encephalitis, with autoimmune encephalitis showing more favorable outcomes than others.
Evidence Rating Level: 2 (Good)
Encephalitis is commonly caused by infectious pathogens, but can also result from autoimmune disorders, toxins, or other diseases. The functional outcomes and long-term recovery following severe encephalitis are not well understood. This study thus aimed to characterize functional outcomes and recovery trajectories through 1 year among adults with encephalitis admitted to the intensive care unit (ICU). This prospective cohort study was conducted across 31 French centers from October 2017 to April 2021 and included adults (>18 years) with probable or confirmed encephalitis requiring ICU care. Causes of encephalitis were split into 4 different categories: infectious, autoimmune, other causes, and unknown origin. The primary endpoint was an unfavorable outcome (severe disability or death) at 3 months, assessed using the modified Rankin scale. Out of the 310 patients were included in the study (median [IQR] age, 60 [43-70] years; 177 male [57.1%]), 123 (39.7%) were diagnosed with infectious encephalitis, 42 (13.5%) with autoimmune encephalitis, 37 (11.9%) with other encephalitis causes, and 108 (34.8%) with encephalitis of unknown origin. At 3 months, 161 patients (51.9%) had an unfavorable outcome, which included 84 deaths (27.1%). Independent factors associated with an unfavorable outcome included age (odds ratio [OR] per 5-year increment, 1.28, 95% CI, 1.16 to 1.41) and immunocompromised status (OR, 3.12; 95% CI, 1.57 to 6.40), while early intravenous acyclovir on the day of ICU admission was associated with a favorable outcome (OR, 0.38; 95% CI, 0.20 to 0.72). From 3 months to 1 year, the proportion of patients achieving functional independence remained unchanged (difference in proportions 1.1%; 95% CI, −6.9% to 9.2%). Patients with autoimmune encephalitis showed improvement through 1 year (difference in proportions, 8.9%; 95% CI, 1.2% to 16.6%), whereas no changes were seen in patients with infectious causes, other causes, or unknown origin. Overall, this study found that about half of adult patients with severe encephalitis requiring ICU care had a poor prognosis at 3 months. Additionally, 1-year recovery trajectories varied by cause of encephalitis, with autoimmune encephalitis showing more favorable outcomes than others. These findings highlight the need for tailored long-term support for patients with encephalitis.
Early Blood Pressure Targets in Acute Spinal Cord Injury: A Randomized Clinical Trial
1. Early augmented blood pressure management did not result in better neurological recovery compared with conventional blood pressure management at 6 months in patients with spinal cord injury.
Evidence Rating Level: 2 (Good)
Although spinal cord injury (SCI) guidelines recommend maintaining higher than normal mean arterial pressure (MAP) for 3-7 days post-injury, they are based on low-quality evidence of neurologic improvement. The impact of early targeted hemodynamic management on long-term neurological outcomes after SCI has not been systematically studied. This study thus compared the efficacy and safety of early blood pressure augmentation vs conventional blood pressure on neurological outcomes after acute SCI. This randomized clinical trial was conducted at 13 large US trauma centers from October 3, 2017, to July 26, 2023, and included patients >18 years with SCI followed up for 6 months. Patients were randomized 1:1 to two groups: augmented blood pressure group (ABP) (target MAP >85-90 mm Hg) or conventional blood pressure (CBP) (target MAP >65-70 mm Hg), with MAP targets maintained for 7 days or until intensive care unit discharge. Primary end points were motor and sensory changes from baseline to 6 months based on scores from the American Spinal Injury Association Impairment Scale. A total of 92 patients were included in this study (mean [SD] age, 53.78 [18.74] years; 76 [83%] male). At 6 months, 38 patients completed follow-up, and 15 had died. Among survivors, there were no mean (SD) differences observed between ABP and CBP groups for change from baseline in upper extremity motor scores (34.95 [3.25] vs 32.95 [3.65]; difference, 2.48; 95% CI, −5.93 to 10.90), lower extremity motor scores (18.53 [4.62] vs 19.95 [4.59]; difference, −4.56; 95% CI, −16.11 to 7.03), or total sensory scores (108.47 [12.49] vs 130.89 [14.87]; difference, −32.00; 95% CI, −65.40 to 1.40). Compared to the CBP group, the ABP group had higher mean (SD) modified Sequential Organ Failure Assessment scores (excluding cardiovascular components) at day 3 (1.65 [1.79] vs 0.80 [1.10]; difference, 0.85; 95% CI, 0.23-1.47) and day 6 (1.55 [1.82] vs 0.80 [1.35]; difference, 0.74; 95% CI, 0.05-1.44), longer mechanical ventilatory support (9.44 [15.27] vs 3.78 [8.42] days; difference, 5.67 days; 95% CI, 0.48-10.85 days), and more respiratory complications (36 [78%] vs 18 [39%]; risk difference, 40%; 95% CI, 22%-58%). There were no differences observed in mortality or other secondary outcomes. Overall, early augmented blood pressure management did not result in better neurological recovery compared with conventional blood pressure management at 6 months in patients with SCI. These findings call into question the practice of MAP augmentation in this population. However, as this study was underpowered, future studies with larger sample sizes are needed to validate these results.
1. Higher adherence to the planetary health diet was associated with lower risk of type 2 diabetes and greenhouse gas emissions.
Evidence Rating Level: 2 (Good)
The rising prevalence of type 2 diabetes (T2D) has been driven by increasing obesity, largely linked to unhealthy diets. The planetary health diet (PHD) has been recommended by the EAT-Lancet Commission on Food, Planet, Health to improve human health and protect the environment. PHD involves eating higher amounts of healthful plant foods and lower amounts of less animal-derived foods. However, the association between the PHD and risk of T2D and diet-related GHG emissions is inconsistent. This study thus examined whether adherence to the planetary health diet was associated with incident T2D and GHG emissions. Data was analyzed from the EPIC-Norfolk prospective cohort study in the UK, which recruited adults aged 40-79. Dietary intake was assessed at baseline (1993–1997) and two follow-up phases (1998–2000 and 2004–2011) using a food frequency questionnaire. Adherence to the PHD was scored by assessing intake of 13 food groups and 2 nutrients. Incident cases of T2D occurring up to March 31, 2020 were analyzed. This study included 23,722 participants (mean [SD] age = 59.1 [9.3] years, 55% female, mean BMI = 26.3 [3.9] kg/m2.), with 3,496 cases of incident T2D recorded over a mean (SD) follow-up of 19.4 (6.8) years. Compared to participants in the lowest PHD quintile (score 33.9–68.4), participants in the highest quintile (score 85.7–117.8) had a lower risk of T2D (adjusted hazard ratio [aHR] [95% CI] = 0.68 [0.61, 0.76]). The estimated population attributable fraction (PAF) for incident T2D due to adherence below the 80th percentile (85.7 points) was 12.3% (95% CI: 9.2%, 15.3%), indicating about 12% of new T2D cases could have been prevented had all participants reached this level. Compared to participants in the lowest PHD quintile, those in the highest quintile had about 18% lower GHG emissions (β5th/1st −18.4%, [95% CI −19.3%, −17.5%]). Overall, this study found that adherence to the PHD was associated with lower incidence of T2D and lower diet-related GHG emissions.
1. Among patients hospitalized with COVID-19, end-stage renal disease was not associated with risk for hospital, non-hospital, or overall death within 180 days post-discharge, but was associated with increased risk of 30-day hospital readmission.
Evidence Rating Level: 2 (Good)
Patients receiving hemodialysis for end-stage renal disease (ESRD) are known to have a high 30-day readmission rate, a pattern also seen for COVID-19-related hospitalizations. Individuals with ESRD hospitalized for COVID-19 may therefore have a higher risk for adverse events after discharge. This study examined whether ESRD is associated with higher risk for death within 180 days or for 30-day hospital readmission among patients hospitalized for COVID-19. This retrospective cohort study used data from the University of California COVID Research Database, covering five California medical centers, and included adults (>18 years) with and without ESRD who were hospitalized for COVID-19 between January 6, 2020, and August 3, 2023, and discharged alive by August 4, 2023. Among the 11,406 patients included in the study, 713 (6.3%) had ESRD. Compared to patients without ESRD, those with ESRD had a higher risk of hospital (hazard ratio [HR] 2.15, 95% CI 1.27–3.63) and overall death (HR 1.49, 95% CI 1.05–2.11) within 180 days post-discharge. However, these results were no longer significant after adjusting for covariates. No association was found between ESRD and risk of non-hospital death within 180 days post-discharge. Patients with ESRD had a higher risk of 30-day hospital readmission, even after adjusting for covariates (adjusted HR 1.36, 95% CI 1.14–1.63). Overall, this study found that ESRD status among patients hospitalized with COVID-19 was not associated with risk for hospital, non-hospital, or overall death within 180 days post-discharge, but was associated with increased risk of 30-day hospital readmission. These findings suggest the need for closer post-discharge follow-up and care coordination in this population.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.