2 Minute Medicine Rewind September 17, 2018
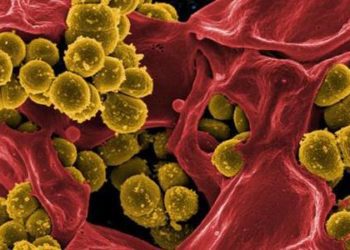
With the rise of gram-negative bacteria producing extended spectrum B-lactamase (ESBL) enzymes, clinicians have turned to carbapenems as the treatment of choice for serious infections caused by these organisms. The overuse of carbapenems, however, has led to increasing carbapenem resistance in gram-negative bacilli. In this randomized controlled trial, 379 hospitalized patients with at least 1 positive blood culture with E. coli or K. pneumoniae testing non-susceptible to ceftriaxone but susceptible to piperacillin-tazobactam were randomized 1:1 to receive intravenous piperacillin-tazobactam (4.5 g) every 6 hours or meropenem (1 g) every 8 hours for a minimum of 4 days, up to a maximum of 14 days to determine whether definitive therapy with piperacillin-tazobactam is non-inferior to meropenem in patients with bacteremia caused by ceftriaxone-non-susceptible E. coli or K. pneumoniae. The primary outcome was all-cause mortality at 30 days after randomization. A noninferiority margin of 5% was used. Researchers found that 12.3% of patients that were randomized to receive piperacillin-tazobactam met the primary outcome of mortality at 30 days compared with 3.7% of the patients randomized to receive meropenem (risk difference 8.6%, 1-sided 97.5% Cl −∞ to 14.5%, p = 0.90 for non-inferiority). Nonfatal serious adverse events occurred in 2.7% of patients in the piperacillin-tazobactam group and in 1.6% of patients in the meropenem group. This study therefore shows that inpatients with E. coli or K pneumoniae bacteremia and ceftriaxone resistance, treatment with piperacillin-tazobactam compared with meropenem did not result in a non-inferior 30-day mortality. The results of this study do not support the use piperacillin-tazobactam in this setting.
Currently, there are two gold standard treatments for acute ischemic stroke: intravenous alteplase (tPA) and endovascular therapy within 6 hours of symptom onset, both of which aim to achieve early recanalization of an occluded intracranial artery. The aim of this multicenter prospective cohort study (n=575) was to examine recanalization over time across a range of intracranial thrombus occlusion sites and clinical and imaging characteristics in patients with ischemic stroke treated with and without intravenous alteplase. The main outcome measured was recanalization on repeat computed tomographic angiography (CTA) or on first angiographic acquisition of affected intracranial circulation obtained within 6 hours of baseline CTA, defined using the revised arterial occlusion scale (rAOL) (scores from 0 [primary occlusive lesion remains the same] to 3 [complete revascularization of primary occlusion]). Two hundred and seventy-five patients (47.8%) received intravenous alteplase only, 195 (33.9%) received intravenous alteplase plus endovascular thrombectomy, 48 (8.3%) received endovascular thrombectomy alone, and 57 (9.9%) received conservative treatment. Successful recanalization occurred at an unadjusted rate of 27.3% overall, including in 30.4% (143/470) of patients who received intravenous alteplase and 13.3%(14/105) who did not with a difference rate of 17.1% (95% CI 10.2% to 25.8%). Among patients that received alteplase, the following factors were associated with recanalization: time from treatment start to recanalization assessment (OR 1.28 for every 30-minute increase in time, 95% CI 1.18 to 1.38, p=0.05), distal thrombus location (i.e. distal M1 middle cerebral artery vs. internal carotid artery) (OR 5.61, 95% CI 2.38 to 13.26), and higher residual flow (thrombus permeability) grade (OR 7.03, 95% CI 3.32 to 14.87). This study therefore shows that in patients with acute ischemic stroke, more distal thrombus location, greater thrombus permeability, and longer time to recanalization assessment were associated with recanalization of arterial occlusion after administration of intravenous alteplase; and among patients who did not receive alteplase, rates of arterial recanalization were low.
Bacteremia is the leading cause of morbidity and mortality in children undergoing hematopoietic stem cell transplantation (HSCT) as part of the management of acute myeloid leukemia (AML) or relapsed acute lymphoblastic leukemia (ALL). The aim of this multicenter randomized trial was to determine the efficacy and risks of levofloxacin prophylaxis in this patient population. As part of this study, patients (age 6 months to 21 years) receiving intensive chemotherapy were enrolled in 2 separate groups: acute leukemia, consisting of acute myeloid leukemia or relapsed acute lymphoblastic leukemia, and HSCT recipients. Patients with acute leukemia were randomized to receive levofloxacin prophylaxis for 2 consecutive cycles of chemotherapy (n=100) or no prophylaxis (n=100). Those undergoing HSCT were randomized to receive levofloxacin prophylaxis during 1 HSCT procedure (n=210) or no prophylaxis (n=214). The primary outcome was the occurrence of bacteremia during 2 chemotherapy cycles (acute leukemia) or 1 transplant procedure (HSCT). Researchers found that, in patients with acute leukemia, the likelihood of bacteremia was significantly lower in the levofloxacin prophylaxis group when compared to the control group (21.9% vs. 43.4%, risk difference 21.6%, 95% CI 8.8% to 34.4%, p=0.001). Among patients undergoing HSCT, however, the risk of bacteremia was not significantly lower in the levofloxacin prophylaxis group (11.0% vs. 17.3%, risk difference 6.3%, 95% CI 0.3% to 13.0%, p=0.06). This study therefore shows that levofloxacin prophylaxis significantly reduces the risk of bacteremia in children with acute leukemia receiving intensive chemotherapy, but not in those undergoing HSCT.
The radial and femoral arteries are typically used as vascular access sites in patients with acute coronary syndrome undergoing invasive management. While there has been recent data indicating that radial access is associated with improved outcomes and quality of life, little is known on the long-term effects of using this site. In addition, the use of bivalirudin compared to unfractionated heparin has been shown to mitigate the risks of bleeding, however, its efficacy on reducing the incidence of long-term ischemic events remains controversial. The Minimizing Adverse Hemorrhagic Events by Transradial Access Site and Systemic Implementation of Angiox (MATRIX) program was designed to assess the safety and effectiveness of radial versus femoral access, and of bivalirudin versus unfractionated heparin in patients with acute coronary syndrome undergoing invasive management. As part of this study, patients with ST-elevation myocardial infarction were randomly assigned before coronary angiography to radial or femoral access and to bivalirudin, with or without post-percutaneous coronary intervention infusion or unfractionated heparin. Patients with non-ST-elevation acute coronary syndrome were randomly assigned before coronary angiography to radial or femoral access and, only if deemed eligible to percutaneous coronary intervention after angiography. Co-primary outcomes for MATRIX access and MATRIX antithrombin type were major adverse cardiovascular events, defined as the composite of all-cause mortality, myocardial infarction, or stroke up to 30 days. Researchers found that at 1 year of follow-up, major adverse cardiovascular events did not differ between patients assigned to radial access compared to those assigned to femoral access (14.2% vs. 15.7%, OR 0.89, 95% CI 0.80 to 1.00, p=0.0526). The net number of adverse clinical events, however, was fewer in the radial access group when compared to femoral access group (15.2% vs. 17.2%, OR 0.87, 95% Cl 0.78 0.97, p=0. 0128). There were no differences in major adverse cardiovascular or net adverse clinical events between heparin and bivalirudin groups. This study therefore shows that in patients with acute coronary syndrome, radial access was associated with lower rates of adverse clinical events compared with femoral access, but not major adverse cardiovascular events at 1 year.
Prevalence of cannabis use in electronic cigarettes among US youth
The use of electronic cigarettes among youth is on the rise. In addition to tobacco products, cannabis and other substances can be used in e-cigarettes. The purpose of this study was to estimate the national prevalence of self-reported cannabis use in e-cigarettes among US middle and high school students. Data was obtained from the 2016 National Youth Tobacco Survey (NYTS), a cross-sectional, school-based study. As part of this study, cluster sampling was used to provide a nationally representative sample of students attending public and private schools. Researchers found that 8.9% (95% CI 8.1% to 9.9%) of all students had used cannabis in e-cigarettes. Among students who had ever used e-cigarettes, cannabis use with e-cigarettes was 30.6% (95% CI 28.3% to 33.1%). Prevalence was significantly higher among male students (p<0.001), high school students (p<0.001), and in individuals that lived with a user of tobacco products (p<0.001). In assessing differences among racial and/or ethnic groups, researchers also found that prevalence of use was higher among Hispanics compared to other groups (p=0.04). This study therefore shows that a significant proportion of school-aged individuals use cannabis through e-cigarettes. This has important implications as cannabis use among youth can adversely affect learning and memory, and therefore, may impair later academic achievement and education.
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.