Perioperative Nivolumab in Resectable Lung Cancer
1. The 18-month event-free survival in the perioperative nivolumab group was 70.2% vs 50.0% in the chemotherapy group with HR 0.58 (significant).
2. Grade 3-4 treatment-related adverse events occurred in 32.5% in the nivolumab group vs 25.2% in the chemotherapy group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Nivolumab, an anti-PD-1 antibody, combined with chemotherapy, has been used as neoadjuvant treatment for resectable non-small-cell lung cancer (NSCLC). Recently perioperative approaches, involving both neoadjuvant and adjuvant immunotherapy, have shown promising results in reducing disease relapse and improving overall survival. This study investigated perioperative nivolumab vs chemotherapy in patients with resectable NSCLC. The primary endpoint was event-free survival (EFS) and secondary endpoints included objective response rate (ORR), quality of life (QoL), and safety. The 18-month EFS was 70.2% in the nivolumab group and 50.0% in the chemotherapy group with HR 0.58 (significant), however in the subgroup with tumor PD-L1 expression of less than 1%, the HR was 0.73 (non-significant). The ORR found pCR occurred in 25.3% in the nivolumab group vs 4.7% in the chemotherapy group with OR 6.64 (significant), and pPR occurred in 35.4% in the nivolumab group vs 12.1% in the chemotherapy group with OR 4.01 (significant). QoL change from baseline was not considered to be clinically meaningful in either group, but time until definitive deterioration in disease-related symptoms was 40.0 months in the nivolumab group vs 31.1 months in the chemotherapy group with HR 0.66 (significant). With regards to safety, grade 3-4 treatment-related adverse events occurred in 32.5% in the nivolumab group vs 25.2% in the chemotherapy group; the most common grade 3-4 event was decreased neutrophil count (10.1% vs 6.5%, respectively). The strengths of this study included its methodology and sample size, and the limitations included lack of overall survival data. Overall, this study found that perioperative nivolumab had some improved outcomes compared to chemotherapy alone in patients with resectable stage IIA to IIIB NSCLC.
Click to read the study in NEJM
Relevant Reading: Perioperative Pembrolizumab for Early-Stage Non–Small-Cell Lung Cancer
In-Depth [randomized controlled trial]: This international, phase III, double-blind study enrolled adults with stage IIA to IIIB NSCLC and randomized them (1:1) to two treatment arms; the nivolumab arm (neoadjuvant nivolumab with platinum-doublet chemotherapy followed by adjuvant nivolumab, n = 229), and the chemotherapy arm (neoadjuvant placebo with platinum-doublet chemotherapy followed by adjuvant placebo, n = 232). Complete neoadjuvant treatment was completed in 84.7% of the nivolumab group vs 88.4% of the chemotherapy group. Definitive surgery occurred in 77.7% of the nivolumab group vs 76.7% in the chemotherapy group, and R0 resection occurred in 89.3% and 90.4% respectively. The median follow-up was 25.4 months. The 18-month EFS was 70.2% in the nivolumab group and 50.0% in the chemotherapy group with HR 0.58 (95%CI, 0.42-0.81, p<0.001), however in the subgroup with tumor PD-L1 expression of less than 1%, the HR was 0.73 (95%CI, 0.47-1.15). The ORR found pCR occurred in 25.3% (95%CI, 19.8-31.5) in the nivolumab group vs 4.7% (95%CI, 2.4-8.3) in the chemotherapy group with OR 6.64 (95%CI, 3.40-12.97), and pPR occurred in 35.4% (95%CI, 29.2-41.9) in the nivolumab group vs 12.1% (95%CI, 8.2-17.0), in the chemotherapy group with OR 4.01 (95%CI, 2.48-6.49). QoL change from baseline was not considered to be clinically meaningful in either group, but the time until definitive deterioration in disease-related symptoms was 40.0 months (95%CI, 33.6-NA) in the nivolumab group vs 31.1 months (95%CI, 25.0-NA) in the chemotherapy group with HR 0.66 (95% CI, 0.45-0.98). With regards to safety, grade 3-4 treatment-related adverse events occurred in 32.5% in the nivolumab group vs 25.2% in the chemotherapy group; the most common grade 3-4 event was decreased neutrophil count (10.1% vs 6.5%, respectively). Overall, this study found that perioperative nivolumab had some improved outcomes compared to chemotherapy alone in patients with resectable stage IIA to IIIB NSCLC.
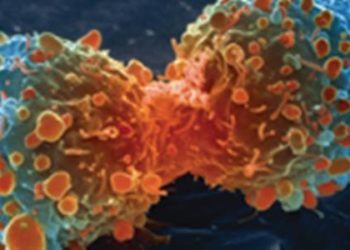
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![Fluorophores enhance visualization for image-guided surgery [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/01/FISH_13_21-350x250.jpg)