Rates of subsequent cardiovascular events similar between ticagrelor and clopidogrel in patients with acute coronary syndrome
1. In this modern population of Canadian patients with acute coronary syndrome (ACS) treated with percutaneous coronary intervention (PCI), the rates of major adverse cardiovascular events (MACE) at 1 year follow-up were the same in groups treated with ticagrelor or clopidogrel. Ticagrelor was linked with a higher risk of major bleeding and dyspnea.
2. Adherence to anti-platelet therapy was linked to lower risk of MACE, though non-adherence was common in both the ticagrelor and clopidogrel groups.
Evidence Rating Level: 2 (Good)
Study Rundown: Current guidelines recommend ticagrelor over clopidogrel along with aspirin as antiplatelet therapy for management of ACS. The recommendations are based on the results of the initial clinical trials such as the Platelet Inhibition and Patient Outcomes (PLATO) trial which demonstrated lower MACE but increased risk of bleeding. The benefit of ticagrelor in a modern cohort of patients undergoing PCI with second generation and later stents is not clear and may expose patients to increase risk of bleeding. The current study sought to evaluate a cohort of patients with ACS undergoing PCI who were prescribed either ticagrelor or clopidogrel. The study found no difference in MACE risk at 1 year follow-up, but ticagrelor was linked with increased risk of major bleeding and dyspnea. Treatment non-adherence was common in both groups and linked to an increased risk of MACE.
This study suggests that modern drug-eluting stents used in PCI may attenuate the benefit seen with ticagrelor in patients with bare metal or first generation stents, or those not managed with PCI. Further randomized trials would be needed to clarify this observation. The main strengths of the study include the large modern cohort with universal access to care and the availability of pharmacy data to estimate drug adherence. The main limitations include the observational design of the study, significant differences between groups prescribed ticagrelor or clopidogrel, and exclusion of outcomes that occurred during the index hospital stay where much of the benefit of ticagrelor may occur.
Click to read the study in JAMA Internal Medicine
In-Depth [prospective cohort]: This study is a prospective cohort design that used data from the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease registry of all patients undergoing PCI in Alberta, and the Pharmaceutical Information Network for data on outpatient transcriptions. Patients were included if they were 18 years or older, underwent PCI for ACS between 2012 and 2016 and filled a prescription for clopidogrel or ticagrelor within 31 days after discharge from index hospital stay. Patients with prescriptions for clopidogrel, prasugrel, or ticagrelor within 120 days prior to the index PCI were excluded. Primary outcome was a composite of all-cause death, hospitalization for ACS, unplanned coronary revascularization, or stent thrombosis within 365 days after index PCI. A total of 13,897 patients underwent PCI during the study period with 11,185 receiving an outpatient prescription for either ticagrelor (36.4%) or clopidogrel (63.6%). There was no significant difference in risk of MACE within 1 year (adjusted hazard ratio [aHR] for ticagrelor, 0.97; 95%CI, 0.85-1.10), but ticagrelor use was linked to increased risk of major bleeding (aHR, 1.51; 95%CI, 1.29-1.78) and dyspnea (aHR, 1.98; 95%CI, 1.47-2.65). Adherence was 73.9% for clopidogrel patients and 81.6% for ticagrelor patients and was linked to lower MACE in both groups (aHR, 0.79; 95%CI, 0.69-0.90).
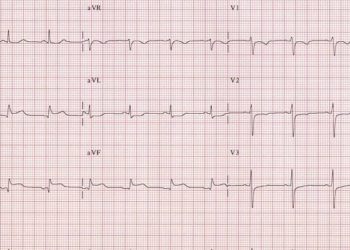
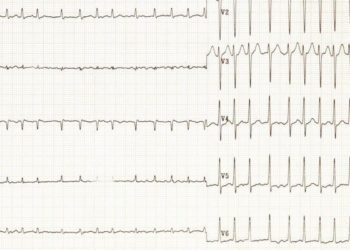
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.