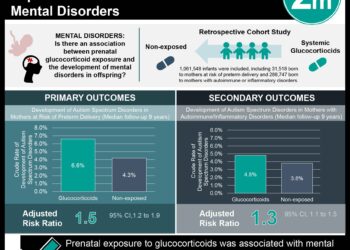
Association Between Immune-Related Adverse Events and Recurrence-Free Survival Among Patients With Stage III Melanoma Randomized to Receive Pembrolizumab or Placebo
1. Immune-related adverse events are associated with a longer recurrence-free survival in patients with stage III melanoma treated with pembrolizumab.
Evidence Rating Level: 1 (Excellent)
Immune-related adverse events (irAEs) occur frequently in patients treated with immune checkpoint inhibitors (ICIs). Retrospective studies and small prospective studies have reported an association between irAEs and improved outcomes in patients with melanoma and lung cancer, suggesting that irAEs may indicate increased drug activity. However, these associations require validation in larger prospective studies with adequate statistical methods. In this secondary analysis of a randomized controlled trial of 1,019 adults with stage III melanoma treated with either pembrolizumab or placebo, 1,011 patients commenced treatment and were studied to investigate the association between irAEs and recurrence-free survival (RFS). At baseline, 61.5% of patients were men, and 62.7% of patients were aged 50 years or older. The median follow-up period was 15 months (IQR 13 to 17 months). Researchers found that the RFS was longer in the pembrolizumab arm compared with the placebo arm (HR 0.56, 98.4% CI 0.43 to 0.74), consistent with the reported main analysis. The incidence of grade 1 or higher irAEs at both 3 months and 15 months was greater in the pembrolizumab group than in the placebo group (3 months: pembrolizumab 19.4%, 95% CI 16.1% to 23.0%; placebo 4.0%, 95% CI 2.5% to 6.0%, 15 months: pembrolizumab 37.4%, 95% CI 33.2% to 41.6%; placebo 9.0%, 95% CI 6.7% to 11.7%; HR 4.95, 95% CI 3.58 to 6.85, p<0.001). The most common irAEs were endocrine disorders and vitiligo. Of those who experienced an irAE, 17.3% patients in the pembrolizumab arm and 13.3% in the placebo arms discontinued treatment due to an irAE. The occurrence of an irAE was associated with a longer RFS in the pembrolizumab arm (HR 0.61, 95% CI 0.39 to 0.95, p=0.03) but not in the placebo arm (HR 1.37, 95% CI 0.82 to 2.29, p=0.21). Moreover, compared with the placebo arm, the reduction in the hazard of recurrence or death in the pembrolizumab arm was greater after an irAE than without or before an irAE (HR 0.37, 95% CI 0.24 to 0.57 vs. HR 0.61, 95% CI 0.49 to 0.77, respectively, p=0.03). Finally, systemic steroid use for irAEs was associated with a higher estimated HR than no steroid use (HR 0.50, 95% CI 0.23 to 1.07 vs. HR 0.34, 95% CI 0.21 to 0.56, respectively). In summary, this study suggests that irAEs are associated with a longer recurrence-free survival in patients with stage III melanoma treated with pembrolizumab.
Click to read the study in JAMA Oncology
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.