Record-based algorithm may improve lung cancer screening follow-up
1. An electronic health record-based trigger algorithm was developed to identify patients with chest imaging results suspicious for malignancy at risk for delayed diagnosis of lung cancer due to a lack of timely follow-up, providing a potential semi-automated method to prevent delayed or overlooked care.
2. The trigger algorithm showed a promising positive predictive value in identifying patients with a prior abnormal imaging result who had not received the appropriate follow-up study while reducing the manual record review burden to less than one-quarter of that necessary to achieve the same result.
Evidence Rating Level: 3 (Average)
Study Rundown: Identifying and preventing delays in cancer diagnosis are challenging. Unfortunately, these delays are common. As many as one-tenth of patients fail to receive a timely follow-up examination, leading to poor outcomes and increased malpractice litigation. While causes of such delays are multifactorial, many arise when records of abnormal screening results are missed by clinicians, due in part to a lack of robust test-result tracking systems, among other reasons. These missed opportunities can result in delays in diagnosis and treatment, and reduce the patient’s ability to receive early, potentially more efficacious therapy. Comprehensive electronic health records (EHRs) that contain longitudinal patient data create an opportunity to automate detection of diagnostic delays and reduce administrative burden. However, use of simple search tools to identify patients with positive test results will likely meet resistance from providers who are already overloaded by the volume of data they receive each day, and lead to a significant loss of time on following-up frequent false positive results. Therefore, proactive, semi-automated or fully automated algorithmic methods are needed to create supportive systems to detect delays in care efficiently. One potential method is the implementation of trigger algorithms to identify specific patterns within the EHR and automatically select a targeted subset of patient records for confirmatory review, thereby improving detection efficiency and reducing the time input necessary. The goal of the present study was to design and assess an automated EHR-based trigger algorithm to identify patients who may suffer significant diagnostic delay following an abnormal chest imaging study. The algorithm identified records of patients who received chest computed tomographic (CT) imaging or conventional radiographs with features which were read as “suspicious for malignancy,” automatically flagging these records to be reviewed for delays in follow-up diagnostic evaluation. The algorithm was applied retrospectively and compared to a manual, thorough record review for validation. This system had a promising positive predictive value (PPV) for the detection of delayed follow-up in the diagnosis of potential lung cancers and laid the foundation for further development of similar detection tools. A significant limitation of this study was that a false positive rate could not be estimated using the data due to the large number of negative records that would need to be reviewed in order to identify a single false negative-result, creating an inability to render sensitivity or specificity data for the trigger algorithm. Additionally, no evaluation was made of patient mortality or morbidity with the use of such an algorithm, leaving out a necessary driver of patient-oriented workflow changes. Future studies aimed at further expanding the use of EHR data-mining to improve patient care are warranted, with particular focus on how such systems may improve such quality indicators as mortality rates.
Click to read the study in Radiology
Relevant Reading: Characteristics and predictors of missed opportunities in lung cancer diagnosis: an electronic health record-based study.
In-Depth [retrospective cohort]: The study included the records of 89 168 patients aged 40-70 seen during a single year at a large Veterans Affairs facility. Subject records were excluded if follow-up to CT and conventional radiographic imaging was performed appropriately within 30 days, or when follow-up was deemed unnecessary, such as in patients with terminal or severe chronic illnesses. Instances of timely follow-up were defined as less than 30 days and may have been by one of many methods, including imaging or clinical visitation. Inclusion criteria required a prior chest imaging study flagged as “suspicious for lung malignancy” by the radiologist, or other “red flag” clinical criteria in patients who were still alive and within the age range necessitating follow-up. The algorithm then identified patients who had the significant inclusion criteria of a suspicious imaging study but who had not received the appropriate follow-up within 30 days, or a group of patients at-risk for delayed diagnosis of lung cancer or loss to follow-up. Descriptive statistics were used to analyze trigger performance, time to follow-up, and cancer outcomes. The final algorithm aimed at detecting an absence of timely follow-up was retrospectively applied to an independent validation cohort to determine the algorithm’s positive predictive value of 57.3%. Of a total of 131 high risk patients identified by the algorithm, 75 of them (57.3%) were true positive, lacking an appropriate follow-up within 30 days, while 56 (42.7%) were falsely positive after manual review, most often due to the suspicious finding being outside of the lungs, such as in the chest wall. As the current study focused on lung cancers specifically, these studies met exclusion criteria, while highlighting the need for careful and specific trigger definitions to further refine such data-mining techniques.
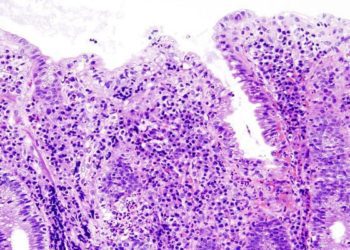
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.