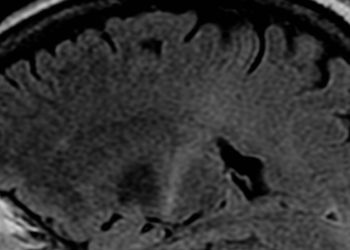
Researchers validate scoring of postconcussive symptom measure to characterize duration
1. After analyzing multiple approaches to the Postconcussion Symptom Inventory (PCSI), researchers found that an increase in severity on 2 or more PCSI items by 1 point or more offered the highest sensitivity in identifying those at risk for prolonged symptomatology.
Evidence Rating: 1 (Excellent)
Study Rundown: Traumatic brain injury (TBI) is a significant pediatric problem, with concussions comprising approximately 90% of all TBIs. Despite a large body of research on the postconcussive pediatric course, there are no clear guidelines on how to best use existing assessment tools in stratifying risk for persistent postconcussive symptoms (PCS). The PCSI is one such tool, which has been validated in children as young as 5 years of age. In the current study, researchers evaluated existing and novel PCSI scoring cutoffs in identifying symptomatic patients at 2 weeks post-injury with clinical judgement as the comparative gold standard. In their assessment of existing cutoffs, they found that a modified version of Zemek et al’s (2013) binary classification system—an increase in severity in 2 or more individual PCSI items by 1 point or more from preinjury to time 2, was the most successful at identifying symptomatic patients. Limitations of this study include using subjective clinical judgement as the comparative baseline to PCSI scores, poor generalizability as the study was completed in the emergency room at a single institution, and recruitment of less than a third of all eligible participants. Overall, this study offers a suggested validated index of pediatric concussion recovery at 2 weeks that may inform physician’s ability to counsel patients on postconcussive course and appropriate timing for returning to daily activities.
Click to read the study, published today in Pediatrics
In-Depth [prospective cohort]: In this single site, prospective, longitudinal study, a total of 1205 pediatric patients between 5-18 years of age were recruited within 48 hours of experiencing an mTBI. Postconcussive symptoms were assessed at time of presentation, at 1 to 4 days post-injury, and 2 weeks post-injury. The primary outcome was presence of PCS determined by applying existing and novel classification systems to parent-rated PCSIs. The PCSI is a 21-item questionnaire that includes cognitive, emotional, physical and sleep-based symptomology questions. The gold standard for comparison was physician clinical judgement. Interrater reliability of clinician assessment of symptomatic/asymptomatic had a ĸ = 0.90, indicating almost perfect agreement between clinicians regarding who was positive or negative for PCS. The authors analyzed the sensitivities of PCSI cutoffs for identifying PCS published by Zemek et al (2013), Barlow et al (2014), and Smyth et al (2015). The Zemek et al criteria had the highest true positive rate (47% identified as positive for PCS, sensitivity = 78.3%). The sensitivities for Smyth et al and Barlow et al were 73.9% and 69.6%, respectively. Area under the curve (AUC) values – or indices of accuracy in distinguishing between PCS and non-PCS patients – for Zemek et al, Smyth et al, and Barlow et al were 0.70, 0.69, and 0.72, respectively. All criteria were significantly better than chance at identifying PCS post-injury. The Barlow et al criteria had the highest diagnostic of OR = 7.0, while Zemek et al had an OR = 5.6, and Smyth et al had an OR = 5.3. The authors novel cutoffs consisted of expanding or decreasing the range of items to be rated for time change in severity. They found that altering the Zemek et al score system to include an increase in severity in 2 or more individual PCSI items by 1 point to increase to 95.6%.
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.