Significant bleeding following percutaneous biopsy is rare
1. In patients who underwent percutaneous biopsy, clinically significant post-procedural hemorrhage is very uncommon, occurring in roughly three per thousand procedures. Delayed pain was the most common compliant following these diagnostic procedures.
2. Percutaneous biopsies of patients on anticoagulant therapy or of native kidneys posed the greatest risk of post-procedural hemorrhage, and in particular, delayed bleeding complications.
Evidence Rating Level: 2 (Good)
Study Rundown: Percutaneous biopsy using ultrasound or CT guidance has become a valuable tool in the minimally invasive acquisition of tissue for pathologic diagnosis. As with all procedures, these are not without risk, with bleeding being the most feared complication following biopsy. While hemorrhages following percutaneous biopsy have been documented in the literature, those studies were limited by their small cohort size and short study period. The goal of the current study was to summarize the timing and clinical presentation of major bleeding events following imaging-guided percutaneous core biopsy in a large sample over an extended study period. Patient records for over 18 000 subjects who underwent percutaneous core biopsies were reviewed and specific information concerning bleeding complications as defined by the Common Terminology Criteria for Adverse Events (CTCAE) were collected to grade hemorrhages from 1-5 based on symptoms. Results revealed that the risk of major bleeding within 24 hours of biopsy was 0.3% overall, and occurred in most frequently in patients undergoing renal biopsy (1.1%). Delayed manifestations of bleeding were found more frequently than predicted, particularly among anticoagulated patients, though not among those on aspirin antiplatelet therapy. An important limitation of this study was that a number of clinically significant hemorrhages secondary to percutaneous biopsy may have been deemed clinically insignificant based on strict adherence to the National Institutes of Health CTCAE guidelines for grading postprocedural bleeds, with those at grade < 3 considered insignificant in this study. Future studies should focus on developing a robust dataset of the risk of post-biospy hemorrhage in an organ specific fashion, and with regard to bleeding risk factors including anticoagulation and various antiplatelet therapies.
Click to read the study in the American Journal of Roentgenology
Relevant Reading: Incidence of bleeding after 15,181 percutaneous biopsies and the role of aspirin.
In-Depth [retrospective cohort]: Clinical information was obtained from 18 947 percutaneous core biopsy reports between September 1, 2005, and May 31, 2012 from a single major academic medical center. Bleeding complication data collected at time points in the 3 months following biopsy were reviewed in accordance with the National Cancer Institute’s CTCAE (version 4.0). Hemorrhages were graded from 1-5 based on symptomatology and the required intervention, with those grade 3 or greater deemed clinically significant, requiring transfusion and/or radiologic, endoscopic or operative intervention. Chart reviews focused specifically on the 64 (0.3%) subjects identified with complications at CTCAE Grade 3 or greater, with data collected regarding timing and clinical manifestation of bleeding. The complaint reported most commonly in this group was pain (61%), and hemorrhage following percutaneous biopsy in the kidney was the most frequent, occurring in 1.2% of those undergoing renal biopsy. The majority of bleeding occurred on the first day following the procedure; with hemorrhages reported at 1 hour (31%), at 2 hours (42%), and at 24 hours (81%). The other 19% of significant bleeding complications occurred after 24 hours of the procedure, which was more than what the authors of this study had anticipated, and was most frequently associated with anticoagulant therapy (unfractioned or low molecular weight heparin or warfarin), but not aspirin antiplatelet therapy.
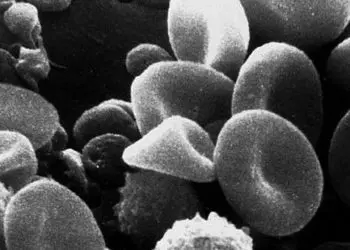
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.



![Reinnervation of cardiac infarcts decreases subsequent arrhythmia incidence [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/02/1280px-Heart_ant_wall_infarction-350x250.jpg)




