Tarlatamab in Small-Cell Lung Cancer after Platinum-Based Chemotherapy
1. Median overall survival was 13.6 months in the tarlatamab group and 8.3 months in the chemotherapy group, with HR 0.60 (significant)
2. Adverse events grade 3 or higher occurred in 54% of the tarlatamab group and 80% of the chemotherapy group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Small-cell lung cancer (SCLC) is challenging to treat in patients with platinum-resistant disease. Tarlatamab, a bispecific T-cell engager targeting DLL3 and CD3, has shown promising results in previous studies. This study evaluated tarlatamab compared to standard chemotherapy in patients with relapsed SCLC after one line of platinum-based therapy. The primary endpoint was overall survival (OS), and secondary endpoints included progression-free survival (PFS) and patient reported outcomes, objective response rate (ORR), and duration of response (DoR). Median OS was 13.6 months in the tarlatamab group and 8.3 months in the chemotherapy group, with HR 0.60 (significant). OS in the tarlatamab group compared to the chemotherapy group was 76% vs 62% at 6 months and 53% vs 37% at 12 months. Median PFS was 4.2 months in the tarlatamab group and 3.7 months in the chemotherapy group. The estimated restricted mean PFS at 12 months was 5.3 months in the tarlatamab group and 4.3 months in the chemotherapy group, with an HR 0.71 (significant). The ORR was 35% in the tarlatamab group vs 20% in the chemotherapy group, with RR 1.73. Median DoR was 6.9 months in the tarlatamab group and 5.5 months in the chemotherapy group. With regards to patient reported outcomes, tarlatamab compared to chemotherapy had a potentially significant decrease in dyspnea and cough. With regards to safety, adverse events grade 3 or higher occurred in 54% in the tarlatamab group and in 80% in the chemotherapy group, with neutropenia (4%) being most common in the tarlatamab group, and anemia (28%) being most common in the chemotherapy group. Cytokine release syndrome (grade 3 or higher) occurred in 1% of the patients and neurologic events (grade 3 or higher) occurred in 4% of the patients in the tarlatamab group. The strengths of this study included the methodology and the limitations included the short follow-up period. Overall, this study found some improvement in outcome measures when treating resistant SCLC patients with tarlatamab compared to standard chemotherapy.
Click to read the study in NEJM
Relevant Reading: Tarlatamab for patients with previously treated small-cell lung cancer
In-Depth [randomized controlled trial]: This multinational, phase 3, open-label study enrolled adults with SCLC who either progressed after first-line platinum treatment, had brain metastasis or both, and randomized them (1:1) to either tarlatamab (n=254) or chemotherapy (n=255). Chemotherapy varied among countries but involved a combination of topotecan, lurbinectedin, or amrubicin. Across the populations, 45% of patients had brain metastases and 44% had platinum-resistant disease. Median duration of follow-up was 11.2 months in the tarlatamab group and 11.7 months in the chemotherapy group. Median OS was 13.6 months (95%CI, 11.1-NA) in the tarlatamab group and 8.3 months (95%CI, 7.0-10.2) in the chemotherapy group, with HR 0.60 (95%CI, 0.47-0.77, p<0.001). OS in the tarlatamab group compared to the chemotherapy group was 76% vs 62% at 6 months and 53% vs 37% at 12 months. Median PFS was 4.2 months (95%CI, 3.4-4.5) in the tarlatamab group and 3.7 months (95%CI, 2.9-4.2) in the chemotherapy group. The estimated restricted mean PFS at 12 months was 5.3 months in the tarlatamab group and 4.3 months in the chemotherapy group (p=0.002), with HR 0.71 (95%CI, 0.59-0.86). The ORR was 35% (95%CI, 29-41) in the tarlatamab group vs 20% (95%CI, 16-26) in the chemotherapy group with RR 1.73 (95%CI, 1.29-2.33). Median DoR was 6.9 months (95%CI, 4.5-12.4) in the tarlatamab group and 5.5 months (95%CI, 4.2-5.7) in the chemotherapy group. With regards to patient reported outcomes, tarlatamab compared to chemotherapy had a potentially significant decrease in dyspnea and cough. With regards to safety, adverse events grade 3 or higher occurred in 54% in the tarlatamab group and in 80% in the chemotherapy group, with neutropenia (4%) being most common in the tarlatamab group, and anemia (28%) being most common in the chemotherapy group. Cytokine release syndrome (grade 3 or higher) occurred 1% of the patients and neurologic events (grade 3 or higher) occurred in 4% of the patients in the tarlatamab group. Overall, this study found some improvement in outcomes measures when treating resistant SCLC patients with tarlatamab compared to standard chemotherapy.
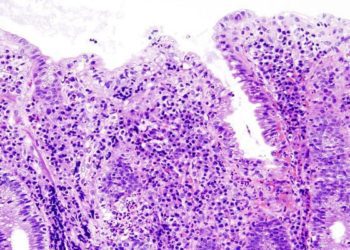
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.