2 Minute Medicine Rewind November 27, 2017
Glucocorticoids are currently recommended as part of the standard of care for patients with Duchenne muscular dystrophy, despite limited understanding of the risks and benefits of glucocorticoid use in this patient population. In this prospective cohort study, investigators followed 440 male patients age 2 to28 years with Duchenne muscular dystrophy in order to analyze the effect of glucocorticoid use on the progression of 9 disease-related mobility and upper limb milestones. Researchers found that patients who had cumulative glucocorticoid treatment for 1 year or longer had significantly longer delays in all disease progression milestones in comparison to patients who were treated for 1 month or never treated (log-rank p<0.0001). In addition, a comparison of patients treated with prednisone or prednisolone with those treated with deflazacort showed that treatment with deflazacort delayed certain disease progression milestones such as age at loss of ability to stand (p=0.0114), age at loss of ambulation (p=0.0102), and age at loss of hand-to-mouth function (p=0.0110). In terms of death, 9% of 311 patients treated with glucocorticoids for 1 year or longer died during follow up, while 19% of patients who had no history of glucocorticoid use died (OR 0.47, 95% CI 0.22 to 1.00, p=0.0501). Overall, results from this study indicate that using glucocorticoids, particularly deflazacort, may delay mobility and upper limb disease progression milestones
Neurocognitive deficits are a common treatment-related adverse effect secondary to radiotherapy or chemoradiotherapy. In this prospective, longitudinal cohort study, investigators followed up 80 patients with head and neck cancer (HNC) and 40 noncancer controls in order to assess neurological function before and after treatment for HNC. Results showed that compared to noncancer controls, patients with HNC demonstrated larger declines in Global Cognitive Function (GCF) composite score at 6 months (Cohen d=-0.38, 95% CI -0.55 to -0.22), 12 months (Cohen d=-0.75, 95% CI -0.92 to -0.58), and 24 months (Cohen d=-1.06, 95% CI -1.26 to -0.86). At 24 months, more patients in the HNC group showed a decline in intellectual capacity (OR 13.0, 95% CI 1.6 to 102.7), verbal memory (OR 9.3, 95% CI 1.1 to 74.9), and executive function (OR 5.8, 95% CI 1.2 to 26.9). Results from this study therefore indicate that HNC survivors are at a higher risk of experiencing treatment-related neurocognitive deficits.
There is current interest in developing new therapies for patients with schizophrenia who experience auditory verbal hallucinations. AVATAR therapy has been proposed as a novel approach that provides patients face-to-face interactions with a digital representation (avatar) of their presumed persecutor and allows therapists to voice this avatar as part of treatment. In this randomized controlled study, investigators randomized 150 patients to either AVATAR therapy or supportive counselling in order to examine the effect of AVATAR therapy on the reduction in auditory verbal hallucinations at 12 weeks. Researchers found that at 12 weeks, there were significantly greater reductions in auditory hallucinations for the AVATAR group than for the supportive counselling group. The AVATAR therapy group had a mean difference of -3.82 (95% CI -6.70 to -0.94, p<0.0093) on the Psychotic Symptom Rating Scales, auditory hallucinations subscale (PSYRATS-AH). For secondary outcomes, the AVATAR therapy group had significantly better outcomes than the control group in terms of the reported frequency of voices (p=0.0013) and reported distress (p=0.017) at 12 weeks. Results from this study suggest that AVATAR therapy has clinical efficacy in reducing persistent auditory verbal hallucinations in patients with schizophrenia. It is important to note, however, that while significant differences were observed at 12 weeks between the two treatment groups, both groups showed comparable improvement on the PSYRATS-AH scale at 24 weeks.
Hybrid Cartilage-Modifying Otoplasty Technique and Outcomes
Otoplasty is a commonly performed procedure for prominauris, a head and neck congenital deformity. It is currently unclear whether hybrid approaches that use cartilage-sparing and cartilage-modifying techniques offer improved safety and efficacy for patients. In this cohort study, investigators reviewed medical records for 23 patients who underwent 24 hybrid cartilage-modifying otoplasty procedures in order to examine the differences between preoperative and postoperative measurements. Results showed that preoperative and postoperative differences were statistically significant for superior (p<0.001), middle (p<0.001), and inferior (p<0.001) helical rim-to-mastoid measurements. Mean decreases for distances were 4.4 mm (SD 2.7 mm), 9.4 mm (SD 3.4 mm), and 5.3 mm (SD 3.6 mm), respectively, for superior, middle, and inferior measurements. In terms of symmetry, the mean postoperative differences between left and right ears for patients who underwent unilateral repair were 1.3 mm (SD 0.8 mm), 3.0 mm (SD 1.2 mm), and 1.0 mm (SD 0.7 mm) for superior, middle, and inferior distances, respectively. For patients with bilateral repair, there were no significant absolute differences for the superior (p=0.41), middle (p=0.58), and inferior (p=0.88) measurements. Overall, results from this study support the efficacy of the hybrid cartilage-modifying otoplasty technique. It should be noted, however, that one surgeon at a single academic center performed these procedures, and as such, further studies are needed to generalize results.
Tuberculosis is a major cause of morbidity and mortality in children infected with the human immunodeficiency virus (HIV). In this observational cohort study, investigators followed 438 HIV-infected children age 13 years or younger with suspected tuberculosis in order to examine the effects of tuberculosis classification and antiretroviral treatment (ART) on mortality. At baseline, 266 out of the 438 children were ART-naïve, and more than half of the children had increased baseline aspartate aminotransferase (AST). Tuberculosis was confirmed in 15% of the children, while another 45% were classified as unconfirmed tuberculosis. Those with a confirmed diagnosis of tuberculosis had a lower 6-month survival probability (65.0%, 95% CI 50.2% to 79.8%) than those with unconfirmed tuberculosis (83.5%, 95% CI 76.8% to 90.3%) or those classified unlikely to have tuberculosis (83.5%, 95% CI 76.3 to 90.7%). Mortality at 6 months was lower in children that had started anti-tuberculosis treatment (p<0.0001). In all three groups, children who died had a higher HIV RNA and AST, and were less likely to have started ART. Multivariate analysis showed that ART initiation during the first month of follow-up (HR 0.08, 95% CI 0.01 to 0.67), confirmed tuberculosis (HR 6.33, 95% CI 2.15 to 18.64), young age (HR 5.90, 95% CI 2.02 to 17.19), CD4 less than 10% (HR 2.63, 95% CI 1.25 to 5.53), miliary features (HR 4.08, 95% CI 1.56 to 10.66) and elevated serum transaminases (HR 4.40, 95% CI 1.82 to 10.65) were all significantly associated with increased mortality. Overall, this study showed that tuberculosis is associated with a high mortality in ART-naïve HIV-infected children, and support the early initiation of ART in cases where there is suspicion of tuberculosis.
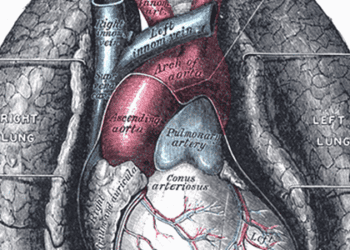
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.