2 Minute Medicine Rewind October 8, 2018
Despite multiple studies indicating that arthroscopic partial meniscectomy (APM) is not more effective than physical therapy (PT), this procedure continues to be performed widely in patients with meniscal tears. In this noninferiority multicenter randomized trial in the Netherlands 321 patients were randomized to APM or a predefined PT protocol to assess whether PT is noninferior to APM in terms of knee function in patients with meniscal tears. The PT protocol consisted of 16 sessions of exercise therapy over 8 weeks focused on coordination and closed kinetic chain strength exercises. The primary outcome was change in patient-reported knee function on the International Knee Documentation Committee Subjective Knee Form (range 0 to 100, from worse to best) from baseline over a 24-month follow-up period. Among the 321 patients who were randomized and followed up over 24 months, knee function improved in the APM group by 26.2 points (from 44.8 to 71.5) and in the PT group by 20.4 points (from 46.5 to 67.7). The overall between group difference was 3.6 points (97.5% Cl -∞ to 6.5, p=0.001 for non-inferiority). Adverse events occurred in 18 participants in the APM group compared to 12 individuals in the PT group. Additional adverse events included repeat surgery (3 in the APM group and 1 in the PT group) and additional outpatients visits for knee pain (6 in the APM group and 2 in the PT group). This study therefore shows that in patients with nonobstructive meniscal tears, PT is noninferior to APM for improving patient-reported knee function over a 24-month follow up period.
There is a strong relationship between body weight and the risk of developing diabetes. Lorcaserin is a selective serotonin 2C receptor agonist that suppresses appetite, and has been shown to sustain weight loss. This randomized double-blind placebo-controlled trial aimed to evaluate the long-term effects of lorcaserin on diabetes prevention and remission. Patients with a BMI of 27 kg/m2 or higher were randomly assigned to receive either lorcaserin 10 mg twice daily, or matching placebo. All patients had access to a standardized weight management program based on lifestyle modification. Researchers found that 56.8% of patients had diabetes, 33.3% had prediabetes, and 9.9% had normoglycemia. At 1 year, diabetic patients treated with lorcaserin had a net weight loss of 2.6 kg when compared to placebo (95% CI 2.3 kg to 2.9 kg, p<0.0001). Prediabetic patients and those with normoglycemia also experienced significant weight loss compared to placebo (p<0.0001). Lorcaserin resulted in a non-significant increase in the rate of achievement of normoglycemia in patients with prediabetes (9.2% vs. 7.6%, HR 1.20, 95% Cl 0.97 to 1. 49, p=0.093). In patients with diabetes at baseline, severe hypoglycemia was rare, but more common in patients treated with lorcaserin (0.4% vs. 0.1%, p=0.054). This study therefore shows that lorcaserin may decrease the risk of incident diabetes and induce remission of hyperglycemia.
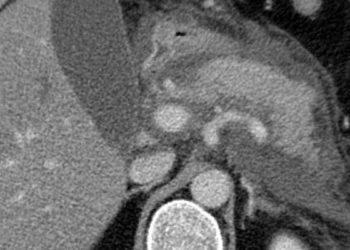
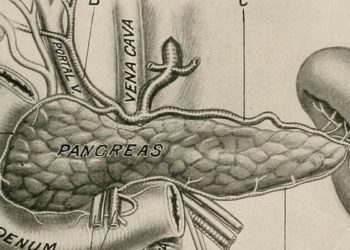
Glucagon-like peptide-1 (GLP-1) potentiates the release of insulin from pancreatic beta cells in a glucose-dependent manner. While pharmacologic studies have shown that GLP-1 delays gastric emptying, reduces appetite, decreases food intake, and therefore, contributes to improved glucose homeostasis and bodyweight, some patients fail to achieve glycemic and bodyweight targets. LY3298176 is a novel dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. Similar to GLP-1, GIP is a potent stimulator of glucose-dependent insulin secretion. In this double-blind randomized phase 2 study, 318 patients with inadequately controlled type 2 diabetes were randomly assigned (1:1:1:1:1:1) to receive either once-weekly subcutaneous LY3298176 (1 mg, 5 mg, 10 mg, or 15 mg), dulaglutide (1.5 mg), or placebo for 26 weeks to assess the efficacy and safety of co-stimulation of the GLP-1 and GIP receptor compared to placebo or selective stimulation of GLP-1 receptors with dulaglutide in patients with poorly controlled type 2 diabetes. Researchers found that at 26 weeks, the effect of LY3298176 on change in HbA1c was dose-dependent and did not plateau; the mean change from baseline in HbA1c with LY3298176 was -1.06% in the 1 mg group, -1.73% for the 5 mg group, -1.89% for the 10 mg group, and -1.94% for 15 mg group, as compared to -0.06% in the placebo group. This corresponded to mean differences of -1.00% (-1.22% to -0.79%) for 1 mg,
-1.67% (-1.88% to -1.46%) for 5 mg, -1.83% (-2.04% to -1.61%) for 10 mg, and -1.89% (-2.11% to -1.67%) for 15 mg. Posterior mean differences for change in HbA1c were also significantly different in the 5 mg (-0.52%), 10 mg (-0.67%) and 15 mg (-0.73%) intervention groups when compared to patients that received dulaglutide. At 26 weeks of follow-up, 33-90% of patients treated with LY3298176 achieved a HbA1c target <7.0% compared to 52% of patients in the dulaglutide group and 12% of patients from the placebo group. In addition, 14-71% of those treated with LY3298176 achieved the weight loss target of at least 5% as compared to 22% of patients in the dulaglutide group and 0% of patients in the placebo group. The 12-week outcomes were like those at 26 weeks for all secondary outcomes. Gastrointestinal events (nausea, diarrhea, and vomiting) were the most common treatment-emergent adverse events in the intervention groups. This study therefore indicates that this dual GIP and GLP-1 receptor agonist shows better efficacy with regard to glucose control and weight loss than dulaglutide and may thus represent a new treatment option in the management of type 2 diabetes.
Fracture Prevention with Zoledronate in Older Women with Osteopenia
Bisphosphonates have been shown to prevent fractures in patients with osteoporosis. However, their role in the prevention of fractures in patients with osteopenia remains unclear. Zoledronate is an appealing option for the prevention of fractures in osteopenia due to its satisfactory safety profile and the infrequency of injections. In this randomized controlled trial, 2000 women with osteopenia age 65 years or older were assigned to receive four infusions of either zoledronate or normal saline at 18-month intervals for 6 years to study the impact on time to first occurrence of a fragility fracture. All participants also received cholecalciferol before and during the trial. Calcium supplementation was not provided. The number of participants who received only one infusion was greater in the zoledronate group than in the placebo group (86 vs. 42, p<0.001). In the zoledronate group, 56 women declined the second infusion due to an acute phase response after the first infusion, whereas only 5 women declined the second infusion for this reason in the placebo group. Researchers found that a fragility fracture occurred in significantly fewer women in the zoledronate group (HR 0.63, 95% CI 0.50 to 0.79, p<0.001). The number of women needed to treat to prevent a fragility fracture in 1 woman was 15. Moreover, compared with women in the placebo group, those in the zoledronate group had a significantly lower risk of experiencing a symptomatic fracture (HR 0.73, 95% CI 0.60 to 0.90, p=0.003) or vertebral fracture (HR 0.45, 95% CI 0.27 to 0.73). There was no significant difference in serious adverse events between the two groups. This study therefore indicates that treatment with zoledronate every 18 months over the course of 6 years may significantly reduce the risk of fragility fractures in women with osteopenia.
Trichomoniasis is the most common sexually transmitted infection among women worldwide. Untreated, this can lead to poor reproductive outcomes and increased rates of HIV transmission. Current guidelines recommend a single 2 g dose of oral metronidazole or tinidazole as first-line treatment, and a 7-day course of oral metronidazole as second-line treatment. However, recent meta-analyses have indicated that a single-dose of metronidazole may be insufficient to cure this disease. In this open-label, randomized controlled trial, 623 women were assigned to receive either a single dose of 2 g metronidazole or 500 mg metronidazole twice daily for 7 days to determine the prevalence of trichomoniasis infection at 4 weeks after completion of treatment. Adherence to treatment was lower in the 7-day-dose group than in the single-dose group (96% vs. 99% respectively, p=0.006). Researchers found that the proportion of women who tested positive for trichomoniasis at 4 weeks was lower in the 7-day dose group than in the single-dose group (11% vs. 19%, RR 0.55, 95% CI 0.34 to 0.70, p<0.0001). The presence of bacterial vaginosis had no significant impact this result (p=0.17 for interaction). There was no significant difference in the proportion of adverse events between the two study groups. However, there were two reported spontaneous abortions among women receiving the 7-day-dose. Limitations of this study included its open-label design and low enrollment. Overall, this study supports the use of a 7-day-dose of metronidazole rather than a single-dose for women with trichomoniasis.
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.