The MR-INFORM trial: fewer patients undergo revascularization when coronary perfusion is assessed with MRI compared to invasive angiography
1. In patients with stable angina and multiple cardiac risk factors, those undergoing myocardial-perfusion cardiovascular magnetic resonance imaging (MRI) compared to invasive angiography and measurement of fractional flow reserve (FFR) underwent fewer coronary revascularization procedures.
2. Patients in the MRI group experienced major adverse cardiac events at a rate non-inferior to the FFR group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Patients with stable angina are treated to reduce the likelihood of adverse cardiac events. Initial management is focused on risk factor reduction or medication use, but if significant coronary perfusion deficits are found revascularization procedures are recommended. Determination of perfusion deficits can be performed using invasive FFR methods or noninvasive MRI techniques, though major studies are lacking comparing the outcomes of patients evaluated by these methods. The Myocardial Perfusion CMR versus Angiography and FFR to Guide the Management of Patients with Stable Coronary Artery Disease (MR-INFORM) trial randomized patients to MRI or FFR groups and found fewer patients in the MRI group underwent coronary revascularization. The composite adverse event outcome of death or other major cardiac events occurring over 1-year following MRI or FFR occurred at a similar rate in both groups.
Strengths of this study include its randomized design, large study size, and evaluation of multiple secondary outcomes, while it is limited by its follow-up extending out to only 1 year.
Click to read the study in NEJM
Relevant Reading: Diagnostic accuracy of stress myocardial perfusion imaging compared to invasive coronary angiography with fractional flow reserve meta-analysis
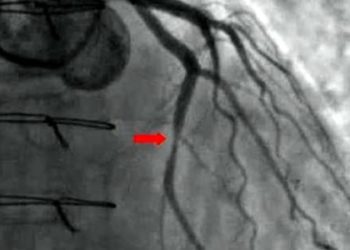
In-Depth [randomized controlled trial]: This international, unblinded, randomized controlled trial enrolled patients between 2010 and 2015. Eligible patients were adults with angina symptoms who had either two or more cardiovascular risk factors or had a positive exercise stress test. Patients with cardiac arrythmias, contraindications to an adenosine MRI, were in heart failure, had a low estimated glomerular filtration rate, had a prior coronary artery bypass graft, or recent cardiac stent were excluded. Randomization into an MRI (n=454) or FFR (n=464) group was done on a 1:1 basis. MRI was performed with a 1.5 Tesla scanner, and recommendation for revascularization for MRI and FFR was done using standard guidelines. In total, 40.5% and 45.9% of patients in the MRI and FFR groups, respectfully, met criteria to recommend revascularization (P=0.11). Patients who underwent index revascularization was lower in the MRI group (162 [35.7%] vs. 209 [45.0%], P=0.005). At 1-year follow-up, the primary safety outcome of a major cardiac adverse event occurred in 3.6% and 3.7% of MRI and FFR patients, respectfully (risk difference, −0.2 percentage points; 95% confidence interval [CI], −2.7 to 2.4; noninferiority margin, 6 percentage points). There was not difference in time-to-first-event between patients in the MRI and FFR groups. Eight revascularization procedures not performed per-protocol based on recommendations occurred in the MRI and FFR groups. Serious adverse events related to perfusion assessment occurred in similar numbers for each group.
Image: PD
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc