ACP releases practice guidelines for the evaluation of suspected acute pulmonary embolism
1. According to the best practice guidelines from the American College of Physicians, clinical risk-stratification tools and sensitive D-dimer tests should dictate use of CT scans to evaluate patients suspected of having acute pulmonary embolism.
2. No imaging should be obtained for patients with D-dimer levels below the normal cutoff, and D-dimer cutoffs should be age-adjusted in patients over the age of 50.
Evidence Rating Level: 1 (Excellent)
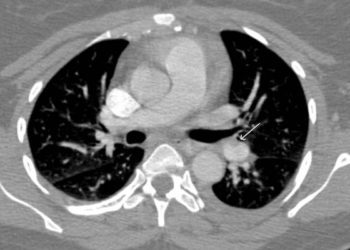
Study Rundown: Acute pulmonary embolism (PE), in which a blood clot blocks blood flow to the lungs, is both common and difficult to diagnose. A number of clinical tools have been created to risk-stratify patients with symptoms of PE, but the best thresholds for testing remain unknown. This guideline from the American College of Physicians aims to provide recommendations for use of two key diagnostic tests—the D-dimer, a non-specific blood test, and a computed tomography (CT) scan of the pulmonary arteries, which can accurately diagnose PE but is associated with non-trivial risks from radiation. Based on an extensive review of literature on PE diagnosis, these guidelines recommend preliminary assessment of a patient’s risk of PE using established risk tools. Patients at intermediate risk of PE based on these tools should undergo D-dimer testing. CT scanning should be reserved for patients who are either at high risk based on risk-assessment tools, or who are at intermediate risk and have elevated D-dimers. The goal of this stratified approach to PE evaluation is to avoid CT scans—and thereby avoid unnecessary radiation—in patients who most likely do not have a PE. Notably, this guideline also includes “clinical gestalt” as an indication for CT scan, although physicians may often have different standards for which factors truly predispose patients to PE. Nevertheless, this guideline carefully combines existing tools with clear and updated recommendations about D-dimer testing and CT scanning, thereby creating a valuable set of diagnostic rules to aid physicians faced with determining which patients do and do not have PEs.
Click to read the policy paper published today in the Annals of Internal Medicine
Relevant Reading: Clinical Decision Rules for Excluding Pulmonary Embolism: A Meta-analysis
In-Depth [clinical best practice guideline]: This best practice guideline builds on other organizations’ existing guidelines for diagnosis of acute PE, as well as on a non-systematic literature review. To identify patients at lowest risk of PE, risk stratification tools, and in particular the Pulmonary Embolism Rule-Out Criteria (PERC), can be applied to identify patients who do not need further workup. For patients who are at intermediate risk based on risk tools (e.g. Wells criteria or the Geneva score) or who do not rule out based on PERC, high-sensitivity D-dimer testing can identify patients who need CT scanning of the pulmonary arteries (CTPA); D-dimer reference ranges should be adjusted for patients over the age of 50. Patients at high risk of PE based on risk-tools should be imaged without D-dimer testing, and ventilation-perfusion scanning should be reserved for patients with contraindications to CTPA. The guidelines also provide a number of insightful recommendations for reducing overuse of CTPA, such as engaging patients in shared decision-making surrounding diagnostic procedures and using electronic clinical decision support to help physicians more closely adhere to evidence-based recommendations.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.