Antiretroviral therapy deferral associated with increased AIDS-defining cancer risk
1. Deferral of antiretroviral therapy was associated with a small increase risk in acquired immunodeficiency syndrome (AIDS)-defining cancers at 10-year follow-up in young, human immunodeficiency virus (HIV)-positive patients.
2. The study was inconclusive on the long-term risk association of early antiretroviral therapy initiation and non-AIDS-defining cancers in the patient population.
Evidence Rating Level: 2 (Good)
Study Rundown: Antiretroviral therapy (ART) is the standard of care for HIV-positive persons. However, there is a gap in knowledge as to whether there is an increased risk of developing cancer due to delays in initiation of ART. This study evaluated the effects of three antiretroviral therapies (ART) treatment strategies on risks for developing non-AIDS defining and AIDS-defining cancer. This study found that the risk for AIDS-defining cancer was slightly higher when ART treatment was delayed compared to when ART treatment was immediately administered. This study was limited by assumptions that there was no unmeasured confounding and that there might be study participants with previously unreported cancer that were included in the analysis. Nonetheless, these study’s findings are significant, as they demonstrate that delaying ART initiation in HIV-positive people is associated with a small increase in risk for AIDS-defining cancer and supports the need for early ART to reduce the risk for developing cancer and for improved early diagnosis and screening of HIV infection in higher-risk populations.
Click to read the study in AIM
Relevant Reading: When to Initiate Combined Antiretroviral Therapy to Reduce Mortality and AIDS-Defining Illness in HIV-Infected Persons in Developed Countries
In-Depth [prospective study]: This prospective cohort study studied 8,318 participants from over 212 clinics in Australia, Europe, and the United States. Patients with at least one CD4 count, at least one positive HIV RNA measurement, free of any cancer, and ART-naive were included in this study. Patients enrolled before 2004 were excluded in this study. The primary outcome for the study was any AIDS-defining and non-AIDS defining cancer. Three treatment strategies utilizing ART were compared: immediate ART initiation, ART initiation after CD4 count < 500 x109 cells/L, and ART initiation after CD4 count < 350 x 109 cells/L. Among the three groups, the risk for non-AIDS-defining cancer and AIDS-defining cancer measured at 10 years of follow-up were 2.97% (95% confidence interval [CI], 2.37 to 3.50) and 2.5% (95% CI, 2.37 to 3.38) respectively for immediate ART initiation. At a CD4 count < 500 x 109 cells/L, the risk of non-AIDS-defining cancer was 3.09% (95% CI, 2.60 to 3.58) and 2.80% (95% CI, 2.37 to 3.38) for AIDS-defining cancer. At a CD4 count < 350 x 109 cells/L, the risk of non-AIDS-defining cancer was 3.27% (95% CI, 2.80 to 3.65) and 3.51% (95% CI, 2.99 to 4.09) for risk of AIDS-defining cancer Furthermore, the risk for any cancer when ART was immediately started was 5.37% (95% CI, 4.63 to 6.19), when ART was started at CD4 count < 500 x 109 cells/L the risk was 5.82% (95% CI, 5.15 to 6.60), and when ART was started at CD4 count <350 x 109 cells/L the risk was 6.65% (95% CI, 5.95 to 7.35). Overall, the study determined delaying ART was associated with an increased risk of developing AIDS-defining cancers.
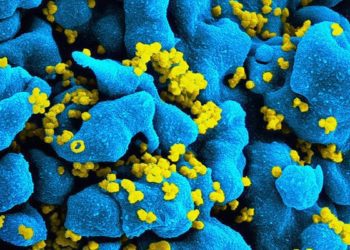
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.