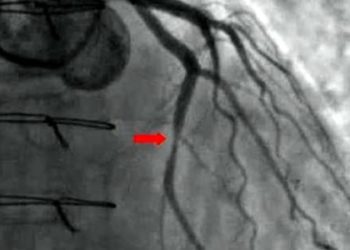
Blood clot prophylaxis for medicine inpatients may be unnecessary
1. Patients who were admitted to the general medicine service for a short stay had a very low risk of developing a blood clot in their veins (venous thromboembolism).
2. Furthermore, the risk of developing a blood clot was not necessarily affected by the receipt of pharmacologic prophylaxis against blood clots at the time of admission.
Evidence Rating Level: 2 (Good)
Study Rundown: Pharmacologic prophylaxis against venous thromboembolism (VTE) has been shown to reduce rates of diagnosed clots, but these studies have mostly been done in surgical or critically ill patients, or in patients that have been admitted to the hospital for over a week. The benefits of this prophylaxis in the general inpatient medicine population admitted for a short stay is not known. This study evaluated whether there is an association between pharmacologic VTE prophylaxis in this lower risk population and the rates of VTE development. The results of the study suggest that the overall risk of developing a VTE in patients admitted on the general medicine wards for a short stay is very low. Furthermore, the addition of pharmacologic VTE prophylaxis in this set of patients did not seem to reduce the rates of VTE.
One of the strengths of the study was the large size of the cohort gathered from many different hospitals, which is much more like a real world scenario. However, since the primary outcome, developing a VTE, was so low, any difference in the benefit of receiving pharmacologic VTE prophylaxis may not have been seen. The biggest weakness of this retrospective observational study was that there were inherent differences between patients receiving pharmacologic VTE prophylaxis compared to those not receiving it. Although the investigators did attempt to control for these confounders, the differences cannot be entirely eliminated.
Click to read the study in JAMA Internal Medicine
Relevant Reading: Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study
In-Depth [retrospective cohort]: The study population consisted of patients who received care at one of the hospitals belonging to the Michigan Hospital Medicine Safety (HMS) Consortium. The inclusion criteria were patients admitted to the general medicine service for a minimum of two days. Patients were excluded if they were receiving systemic anticoagulation for any reason. The primary outcome was VTE development within 90 days of admission that was diagnosed clinically and confirmed with imaging. As a result, only clinically relevant VTEs were included in this analysis. Patient data were collected from January 2011 to December 2012 from 35 hospitals.
A total of 20,794 patients were included in the analysis, of which 14,563 (70%) received pharmacologic VTE prophylaxis. Several VTE prophylaxis regimens were deemed acceptable, including those using heparin, enoxaparin, dalteparin, or fondaparinux. The median length of stay in the hospital was four days. Hospitals were stratified according to high, moderate, or low performance, where pharmacologic VTE prophylaxis use was 85.8%, 72.6%, and 55.5% respectively. There were a total of 226 VTEs identified during the 90-day follow up period. The risk-adjusted hazard of developing a VTE did not differ based on receipt of pharmacologic VTE prophylaxis on hospital admission (HR 1.09; 95% CI, 0.80-1.48). The characteristics that seemed the carry the greatest risk for developing a VTE included hospital stay ≥ 5 days (HR 2.07; 95% CI, 1.58-2.71) and the presence of a central venous catheter (HR 2.86; 95% CI, 2.11-3.87).
More from this author: Chest pain may be better than EKG, echo for predicting coronary artery disease prognosis, Strict blood pressure control in kidney disease linked to worse outcomes, Catheter thrombolysis + anticoagulation may be inferior to anticoagulation alone in DVT, Pediatric brain injury unlikely with isolated loss of consciousness, Ultrasound, flow reserve guided coronary interventions provide minimal benefit
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.

![siRNA against antithrombin alleviates symptoms of hemophilia [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/04/clot-CCWiki-350x250.jpg)