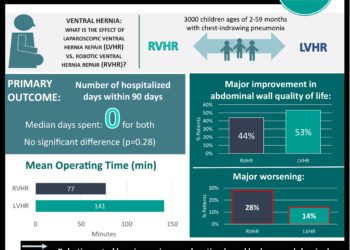
Complications 4.5x more frequent in hernias repaired laparoscopically vs. open repair
[tabs tab1=”2MM Rundown” tab2= “2MM Full Report”]
[tab]
Image: PD
1. Perioperative complications occur in 9% of patients undergoing laparoscopic repair of ventral incisional hernias vs. only 2% in open repairs.
2. Recurrence rate was similar between laparoscopic and open repairs.
3. Median blood loss and number of patients receiving wound drains were higher in open repairs.
4. Median length of stay was 3 days for both procedures.
This randomized clinical trial is the largest to date comparing laparoscopic vs. open ventral incisional hernia repair. For the most part, it reaffirmed previous findings on the outcomes of each procedure. For laparoscopic repair, this means less intraoperative blood loss. However, although some studies previously reported shorter lengths of stay, this study did not find a statistically significant difference for length of stay between the 2 groups. The authors’ finding of longer operative time for laparoscopic procedures is contrary to the findings of prior prospective studies, which have varied in observing laparoscopic procedures to be shorter or of equal operative time. The authors’ claim that the longer laparoscopic operative times are likely due to extensive adhesiolysis of the abdominal wall is reasonable, especially given that 100 minutes for the average procedure is still within a normal range. Lastly, some prior studies reported benefits to laparoscopic repair in perioperative complications, but this study found a statistically significant difference, with laparoscopic repairs yielding relatively more complications, especially intraoperatively.
Lack of segmentation of data according to surgeon’s experience in laparoscopic procedures is a limitation of this study, as it is possible that the differences discovered in this trial may be narrower or nonexistent with surgeons that have more experience with laparoscopic procedures. This detail could affect both operative time and complications. Moreover, while the study notes that mesh placement was mandatory, not having the breakdown of outcomes by mesh placement also limits the generalizability of the data. It is possible that mesh position could affect results. The authors did point out, however, that a Cochrane review yielded insufficient evidence as to which mesh position is best.
Click to read the study in JAMA Surgery
[/tab]
[tab]
Image: PD
1. Perioperative complications occur in 9% of patients undergoing laparoscopic repair of ventral incisional hernias vs. only 2% in open repairs.
2. Recurrence rate was similar between laparoscopic and open repairs.
3. Median blood loss and number of patients receiving wound drains were higher in open repairs.
4. Median length of stay was 3 days for both procedures.
This [randomized] study analyzed 206 patients across 10 hospitals who had previously undergone a laparotomy and developed a ventral incisional hernia requiring repair. The study recorded outcomes for postoperative pain, complications, length of hospital stay, recurrence, morbidity and mortality. 99 patients were randomized to receive laparoscopic repair and 107 were randomized to receive open incisional hernia repair. After randomization, there was no statistically significant difference in any of the patient characteristics recorded. More patients had intraoperative complications in the laparoscopic group, with 9% of patients suffering a complication, (versus 2% in open repairs, P <.05) more than half of which were enterotomies.
Open repairs had more blood loss (50 mL vs. 10 mL, P= 0.05) and were more likely to require wound drains (45% vs. 3%, P = 0.001) than laparoscopic repairs. Median length of stay for both groups was 3 days. Postoperatively, 35% of laparoscopic patients suffered complications compared to 26% of open repair patients, but this difference was not statistically significant. Visual analog scale scores for post-operative pain and nausea were comparable in both groups. Recurrence rates by the mean 35 month follow-up was 18% in laparoscopic patients and 14% in open repair patients, but the difference was also not statistically significant.
In sum: This randomized clinical trial is the largest to date comparing laparoscopic vs. open ventral incisional hernia repair. For the most part, it reaffirmed previous findings on the outcomes of each procedure. For laparoscopic repair, this means less intraoperative blood loss. However, although some studies previously reported shorter lengths of stay, this study did not find a statistically significant difference for length of stay between the 2 groups. The authors’ finding of longer operative time for laparoscopic procedures is contrary to the findings of prior prospective studies, which have varied in observing laparoscopic procedures to be shorter or of equal operative time. The authors’ claim that the longer laparoscopic operative times are likely due to extensive adhesiolysis of the abdominal wall is reasonable, especially given that 100 minutes for the average procedure is still within a normal range. Lastly, some prior studies reported benefits to laparoscopic repair in perioperative complications, but this study found a statistically significant difference, with laparoscopic repairs yielding relatively more complications, especially intraoperatively.
Lack of segmentation of results according to surgeon’s experience in laparoscopic procedures is a limitation of this study, as it is possible that the differences discovered in this trial may be narrower or nonexistent with surgeons that have more experience with laparoscopic procedures. This detail could affect both operative time and complications. Moreover, while the study notes that mesh placement was mandatory, not having the breakdown of outcomes by mesh placement also limits the generalizability of the data. It is possible that mesh position could affect results. The authors did point out, however, that a Cochrane review yielded insufficient evidence as to which mesh position is best.
Click to read the study in JAMA Surgery
By David Mattos and Allen Ho
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.
[/tab]
[/tabs]