Intensive blood pressure control not linked to changes in cerebral perfusion in patients with cerebral small vessel disease
1. In patients with severe cerebral small vessel disease, a strategy of intensive blood pressure control did not significantly alter whole brain blood flow when compared to standard blood pressure control.
Evidence Rating Level: 2 (Good)
Study Rundown: Cerebral small vessel disease (SVD) is a common cause of ischemic stroke and vascular cognitive impairment. Low Cerebral blood flow (CBF) has been linked to increase in white matter hyperintensities (WMH) on visible on MRI, thought to be evidence of a causal relationship between CBF and small vessel disease. While intensive management of systemic hypertension has been shown to decrease incidence of cardiovascular and cerebrovascular outcomes, there has been concern that due to derangements in cerebral vessel autoregulation aggressive lowering of blood pressure may worsen cerebral perfusion in patients with SVD. The current study evaluated whole brain cerebral blood flow (CBF) using MRI measurements in patients with SVD randomized to standard or intensive blood pressure control. The study found that after three months of hypertension management there was no significant differences in global cerebral perfusion, or adverse events.
The study provides evidence towards the safety of intensive blood pressure control strategy in patients with cerebral small vessel disease. The main strengths of the study include the randomized design and intention-to-treat analysis, and there are plans for ongoing assessment up to two years of follow up. The main limitations of the investigation include the absence of updated technology for cerebral perfusion assessment that became available after the study’s original design, small population studied, and its radiographic rather than clinical primary outcome.
Click to read the study, published in JAMA Neurology
Relevant Reading: Patterns of blood pressure response during intensive BP lowering and clinical events: results from the secondary prevention of small subcortical strokes trial
In-Depth [randomized controlled trial]: The PRESERVE study is an ongoing, 2-year multicenter randomized control trial investigating standard (target SBP 130-140 mmHg) versus intensive (SBP <125 mmHg) blood pressure control. The current study is a planned sub-analysis of CBF at 3 months after initiation of therapy. Patients were included if they had MRI-confirmed lacunar stroke and grade 2 or higher WMH, and hypertension. Participants were excluded if they had an acute stroke within 3 months prior to enrolment. The primary endpoint of whole brain CBF was analyzed with MRI using arterial spin labeling.
Of the 62 patients enrolled in the study, 33 in the standard treatment arm, and 29 in the intensive arm had CBF data available at 3 months of follow up. The mean (SD) blood pressure difference was 8 (12)/4(9) mmHg in the standard group, and 27(17)/13(13) mmHg in the intensive group. The change in whole brain CBF was not different between the two study groups: −0.5 (9.4) mL/min/100 g in the standard group vs 0.7 (8.6)mL/min/100g in the intensive group, p = 0.63). There was no difference in adverse events between the study arms (mean events 0.21 vs. 0.32, p = 0.44).
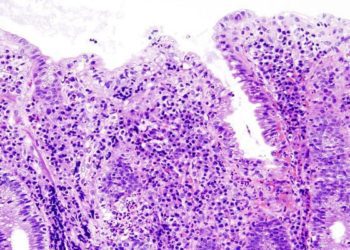
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.