Longer onset-to-treatment time for subarachnoid hemorrhage is associated with increased 12-month all-cause mortality
1. Treatment delay beyond 12.5 hours after the onset of symptoms of subarachnoid hemorrhage (SAH) was associated with increased discharge to rehabilitation, compared to discharge home, a proxy for poorer functional outcomes.
2. Treatment delay beyond 12.25 hours after the onset of symptoms of SAH was associated with increased 12-month all-cause mortality.
Evidence Rating Level: 2 (Good)
Study Rundown: Subarachnoid hemorrhage (SAH) is a significant cause of mortality. The time to intervene for optimal outcomes is poorly understood because of the exclusion of some categories of patients (poor grade or transfers), studies being conducted at only one center or on only one treatment, and the risk of bias in defining ‘early’ and ‘delayed’ treatment. This study attempts to identify the optimal treatment window for the best outcomes after an aneurysmal SAH. Outcomes for this study were defined as the rate of discharge home (compared to rehabilitation service, another hospital, or nursing home), the 12-month survival rate, and the occurrence of any complications (re-bleed, post-treatment stroke, delayed cerebral ischemia or injury, meningitis, seizure, or hydrocephalus). This study, the Reducing Delays in Aneurysmal Subarachnoid Hemorrhage (REDDISH) study, identified cases of SAH to compare their outcomes by onset-to-treatment time. The onset-to-treatment time was defined as the time between the onset of symptoms and the start of neurosurgical or endovascular treatment. Treatment was started an average of 19.37 hours after SAH symptom onset for the 482 enrolled patients. Longer onset-to-treatment time was associated with discharge to a rehabilitation center, compared to discharge home. It was 10% more likely that a patient would go home if treatment occurred within the first 12.5 hours of symptoms. 16% of the participants died at the hospital while 83.0% lived 12 months after their SAH. Longer onset-to-treatment time was associated with increased 12-month all-cause mortality, with the point of minimum mortality occurring with treatment within 12.25 hours. Longer onset-to-treatment time was not associated with an increased risk of complications. A strength of this study was how it features multiple centers and SAH grades, making the results more generalizable to all SAH. One limitation is that for 47 patients their event time data was missing so this study used the time of ambulance call or hospital arrival, which will underestimate the onset-to-treatment time. One major limitation of this study is that it used a proxy of discharge location for functional outcomes, which could lead to misclassification of outcomes: for example, while someone was discharged home, they may be bedbound. Finally, because this study excluded patients who did not even receive treatment, it cannot comment on survivorship rates of SAH admission patients.
Click to read the study in JAMA Network Open
Relevant Reading: Treatment delay from aneurysmal subarachnoid hemorrhage to endovascular treatment: a high-volume hospital experience
In-Depth [retrospective cohort]: This study compared the outcomes based on the onset to treatment time of all aneurysmal SAH patients admitted to 2 Australian cerebrovascular treatment centers. Onset-to-treatment time was compared continuously to the chance of discharge or 12-month survival with multivariable logistic regression or multivariable Cox proportional hazards regression, respectively. 482 patients (age = 55.0±14.5 years, 69.9% female) were treated with neurosurgical or endovascular treatment. The average time to start treatment was 19.37 hours. Out of all the enrolled patients, 41.3% were discharged to rehabilitation and 42.8% were discharged home. Treatment delay was associated with discharge location (rehabilitation vs home) (χ2 test, P = 0.002) even after correcting for sex, treatment modality, severity, Charlson Comorbidity Index, history of hypertension, and hospital transfer. Specifically, the chance of being discharged home increased by 10% if treatment occurred within 12.5 hours of symptoms, while between 20 and 60 hours the chance of discharge home decreased. 16% of the participants who received treatment died from SAH while in hospital. Overall, 83.0% of participants were alive 12 months after their SAH. 81.7% of the deaths due to SAH occurred within 30 days of symptoms. Delay to receiving treatment for SAH was associated with 12-month all-cause mortality (χ2 = 14.39, P = 0.01). The point on the curve of minimum mortality occurred when receiving treatment at 12.25 hours after symptoms arose. Participants were 4 times as likely to die if treatment was received 24 hours after symptom onset compared to within 12.25 hours. This association was attenuated but largely similar when correcting for sex, age, treatment modality, severity, comorbidities, and hospital transfer. Greater than 50% of participants experienced a complication. Treatment delay was not associated with an increased risk of complications. Sensitivity analysis focused only on those actively treated within 72 hours and were consistent with these results.
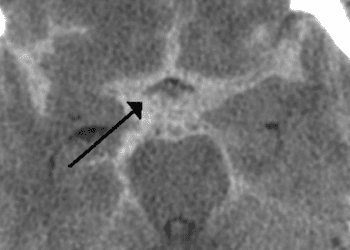
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-350x250.jpg)