Most children needing end-of-life care receive it in acute care settings
1. In this retrospective study, the majority of children studied died of chronic conditions or congenital illnesses in institutional settings (intensive care unit [ICU], emergency department [ED], or non-ICU institution).
2. Health care costs increased most notably during the last 5 months of life, more than doubling for children who died of congenital or perinatal and chronic illnesses.
Evidence Rating: 2 (Good)
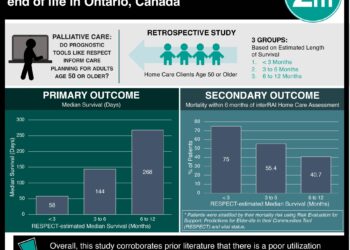
Study Rundown: The American Academy of Pediatrics (AAP) has previously called for greater availability and accessibility of palliative care and respite programs for children living with life-threatening or terminal conditions. For state agencies, policy makers, and health plans, a challenge to addressing this recommendation includes the limitedness of expenditure information on health care for children with life-limiting conditions. In this study, researchers aimed to provide such baseline data by evaluating the location, cause of death, and health care use and costs over the last year of life for children ages 1 month to 19 years who died in Ontario, Canada. In terms of location, the majority of pediatric deaths occurred in an institutional setting. Of note, at the time of the study, there was no freestanding pediatric hospice available. Additionally, researchers found that the majority of costs were incurred in an acute care setting, and costs increased most dramatically during the last 5 months of life, particularly for children with congenital/perinatal and chronic medical conditions. While the study provides excellent baseline data on end-of-life health care expenditures, the authors acknowledge that there is no evaluation of quality of care and decision-making analysis regarding health care use. Additionally, the costs of freestanding hospice paid through philanthropic support were not able to be included in this analysis. The results of these studies may only be generalizable to other countries with similar health care systems to Canada (e.g. England). The authors recommend further research to better understand the role of palliative care services in optimizing care and cost.
Click to read the study, published today in Pediatrics
In-Depth [retrospective cohort]: A total of 1620 children aged 1 month to 19 years who died in Ontario, Canada were evaluated in this study conducted from April 1, 2010 to March 31, 2013. Infants <30 days of age at time of death were excluded, due to frequent lack of health care card numbers resulting in missing data. In terms of demographics, deaths in this cohort tended towards male sex compared to female sex (969 vs. 651, respectively), and the majority of deaths occurred in the 15 to 19-year-old group (37.6%). The majority of children died in institutional settings (75.9%). Specifically, 580 (35.8%) of children died in an ICU, 501 (30.9%) died in an ED, 14 (9.1%) died in a non-ICU institution, and 391 (24.1%) died in a “noninstitution.” The most common cause of death was a chronic condition, demonstrated in 674 (41.6%) of patients, followed by external causes of death in 553 (34.1%) patients, perinatal/congenital causes in 234 (14.4%) patients, and other causes of death (e.g. sudden infant death syndrome) in 137 (8.5%) patients. The mean health care cost during the last year of life for a child was $78 332 CAD, with a total annual cost of $124 million. The bulk of these costs were generated from the acute care sector (75%). The highest mean cost of care came from children with a perinatal/congenital cause of death (mean = $103 472; median = $103 472), followed by children with a chronic condition (mean = $112 623; median = $63 101), other cause of death (mean = $13 599; median = $2037) and external cause of death (mean = $13 071; median = $1963). In general, researchers found that mean costs per child tended to increase over the last 4 months of life, more than doubling for children with perinatal/congenital and chronic conditions.
Image: CC/Wiki/Eyone ambulance emergency
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.