Neurocognitive deficits in congenital heart disease may not worsen with age
1. Although children with congenital heart disease (CHD) performed worse than matched controls on intelligence assessments at ages 4 and 7, relative improvement was observed at age 7.
2. Motor coordination, working memory, inhibition, and cognitive flexibility were not significantly different between children with CHD and matched controls at the examined time points.
Evidence Rating Level: 3 (Fair)
Study Rundown: As medical techniques for treating CHD have advanced, more children are surviving into adulthood. Due partly to their underlying genetic defect, surgery in infancy, and environmental influences, children with CHD are at greater risk of having neurocognitive deficits than those who do not have CHD. Previous work has suggested that neurocognitive functioning in children with CHD may decline with age due to increasing cognitive demands, a phenomenon known as “growing into deficit” (GID), but longitudinal data with matched healthy controls has been scarce. To investigate whether children with CHD would exhibit worsening function compared to age-matched controls, the GID study assessed neurocognitive function in a subset of children who had enrolled as infants in the Leuven glucose control trial (LGC-trial). Children with CHD performed significantly worse on intelligence quotient (IQ) tests at ages 4 and 7 but showed relative improvement at the second time point. Alertness, while significantly worse at age 4, was comparable to that of controls at age 7. Motor coordination, inhibition, and cognitive flexibility were not significantly different between groups at the studied time points. Though limited by its lack of an objective imaging correlate (e.g., magnetic resonance imaging (MRI)) and inability to assess the impact of prior enrollment and treatment in the LGC-trial, the finding of persistent neurocognitive deficits at age 7 in children with CHD coupled to evidence of catch-up on some metrics, warrants continued clinical monitoring and further investigation into possible interventions to further narrow the gap.
Click to read the study, published today in Pediatrics
Relevant Reading: Neurodevelopmental outcomes in children with congenital heart disease: evaluation and management
In-Depth [case-control study]: Participants in the GID study included 100, 7-year olds with CHD and 72 healthy matched controls. The children with CHD were a subset of individuals in the LGC-trial, identified in the pediatric intensive care unit of the University Hospitals Leuven, Belgium following heart surgery. At ages 4 and 7, general intellectual functioning was measured by the Dutch version of the Revised Wechsler Preschool and Primary Scale of Intelligence (WPPSI-R), visual-motor integration (VMI) was assessed by the Beery-Buktenica Developmental Test of Visual-Motor Integration, and attention, motor coordination, and executive functions were tested by 4 computerized tasks of the Amsterdam Neuropsychological Tasks. Psychosocial functioning was assessed (Child Behavior Checklist (CBCL)), as well. The significance of group (CHD vs. control), time (age 4 vs. age 7), and the change over time in each group were examined, with the hypothesis that greater neurocognitive deficit would be observed with increasing age. Although total IQ score remained lower at age 7 in the CHD group compared to children without CHD, the gap separating the groups diminished from 11.7 IQ points at age 4 to 7 points difference at age 7 (interaction p = 0.003). VMI was significantly worse in the CHD group (p < 0.001), and there was no improvement seen in this skillset by age 7 (interaction p = 0.207). Psychosocial function across all measures appeared to be worse at age 7 compared to age 4 in both children with CHD and healthy controls (although different age-appropriate checklists were used); however, only the CBCL-total problems metric was significantly worse in the CHD group compared to controls (p = 0.013)—CBCL-internalizing and CBCL-externalizing problems trended toward significance.
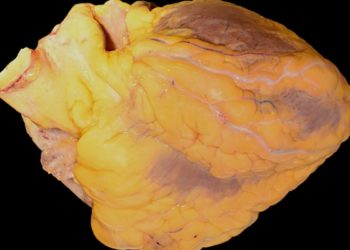
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.