Patient Basics: Absence Seizures (Petit Mal Seizures)
Originally published by Harvard Health.
What Is It?
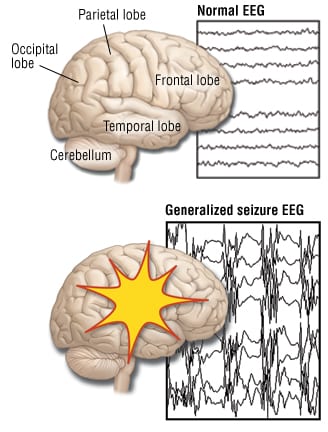
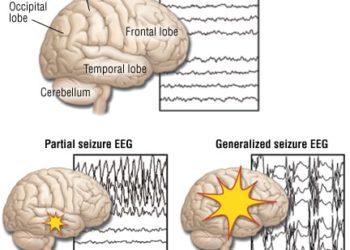
The brain’s nerve cells (neurons) communicate by firing tiny electric signals. During a seizure (convulsion), the firing pattern of these electric signals suddenly changes. It becomes unusually intense and abnormal.
A seizure can affect a small area of the brain. Or it can affect the entire brain. If the whole brain is involved, it is called a generalized seizure.
The two most common forms of generalized seizures are:
- Generalized seizures (grand mal seizures)
- Absence seizures (petit mal seizures)
Both forms of generalized seizures cause a temporary loss of consciousness.
An absence seizure causes a loss of consciousness for 30 seconds or less. It is barely noticeable, if at all. The person simply stops moving or speaking. He or she stares straight ahead blankly, and does not respond to questions. The seizure is short and hard to notice. A person can have 50 or 100 absence seizures a day, without them being detected.
When the absence seizure ends, the person goes back to his or her normal activities. He or she does not realize that anything has happened.
Epilepsy is a brain disorder that causes recurrent seizures if it is not treated. A child with repeated absence seizures is said to have childhood absence epilepsy or petit mal epilepsy.
Absence epilepsy can begin at any time during childhood. Most often it starts between the ages of 4 and 15 years.
In most cases, the reason for the seizures is unknown. Genetic (inherited) factors may play some role in the development of absence epilepsy.
Symptoms
During an absence seizure, a child is temporarily unaware of what is happening around him or her. For a few brief seconds, the child stops what he or she is doing. He or she stares straight ahead and does not respond to people speaking.
During a seizure, a child’s eyelids may blink or flicker very quickly. Or an arm or a leg may twitch, jerk or move for no obvious reason.
After the seizure ends, the child has no memory of the episode. He or she usually resumes previous activities as if nothing happened. There usually is no confusion or recovery period after an absence seizure.
A child with absence epilepsy can have many brief seizures during a school day. As a result, the disorder may interfere seriously with their ability to pay attention and participate in class. For this reason, a teacher may be the first adult to notice that something is wrong. If the teacher is not familiar with absence seizures, he or she may complain that the child is not paying attention or appears to be daydreaming.
Outside the classroom, the child’s symptoms may affect the ability to concentrate when he or she plays sports or does homework. Seizures also may interrupt conversations with friends or family members.
Diagnosis
The doctor will ask you to describe your child’s symptoms. He or she will ask how often the symptoms occur and how long they last. The doctor also will ask whether any other members of your family have had similar symptoms or have received treatment for any type of epilepsy.
The doctor will review your child’s medical history, including:
- Any history of birth trauma
- Serious head injury
- Infections involving the brain, such as encephalitis or meningitis
The doctor will do a thorough physical exam. This will include a complete neurologic examination of your child.
Routine blood tests may follow. These will check for common medical illnesses that either can mimic epilepsy or trigger seizures. In most cases, the results of your child’s physical exam and blood tests will be normal.
As a final step in the diagnostic process, your doctor may order an electroencephalogram (EEG). An EEG is a painless test. It detects the electrical activity in your child’s brain and translates it into a series of printed patterns. In many children with absence epilepsy, the EEG shows a specific pattern that confirms the diagnosis.
In some cases, your child’s doctor may be concerned that the absence seizures are related to a structural abnormality as well as electrical abnormality of the brain. The doctor may order a magnetic resonance imaging (MRI) test or a computed tomography (CT) scan of your child’s brain. Reasons for doing an imaging test include:
- Prolonged seizures
- An unusual pattern of symptoms
- Abnormal findings on the physical or neurological examination
- A condition that would put the child at higher risk of seizures, such as:
- Birth trauma
- Head injury
- Encephalitis
- Meningitis
Expected Duration
Most children outgrow absence epilepsy, usually by their teen years. Before then, anti-epilepsy medication is used to control the symptoms.
Prevention
Absence epilepsy cannot be prevented.
Treatment
If your child has absence epilepsy, the doctor will treat the condition with medication to help control the number of absence seizures your child has. They are known as anticonvulsants (also called antiepileptic or antiseizure drugs).
The two most commonly prescribed anticonvulsant medications to treat absence epilepsy are ethosuximide (Zarontin) and valproic acid (Depakene, Depakote). Ethosuximide only prevents absence seizures. Valproic acid is a general anticonvulsant that also is the treatment for tonic-clonic (grand mal), myoclonic and partial seizures as well as absence seizures.
Controlling absence epilepsy can help your child reach his or her full potential at school and home. Once your child begins taking a seizure medicine, treatment usually continues for at least two years.
When To Call a Professional
Call your child’s doctor if you notice that your child has:
- Staring spells
- Brief periods of deep daydreaming
- Other behaviors that may be symptoms of absence seizures
If your child’s teacher complains that your child is not paying attention, tunes out or always daydreams, ask the teacher whether your child shows other symptoms of absence seizures. For example, does your child:
- Stare straight ahead at the chalkboard
- Blink repeatedly
- Twitch while daydreaming
Request that the teacher write down a detailed description of your child’s symptoms. Have the teacher estimate how long each episode lasts and the number of episodes per day.
Once you have this description, check to see whether you notice any of these same behaviors at home. Then call your doctor to discuss the situation.
Prognosis
The outlook is very good. Most children with absence epilepsy eventually outgrow the condition without complications. With proper treatment, the child can have a normal life at school and at home.
In most cases, there is no long-term effect on brain development, brain function or intelligence.
Additional Info
National Institute of Neurological Disorders and Stroke
P.O. Box 5801
Bethesda, MD 20824
Phone: 301-496-5751
Toll-Free: 1-800-352-9424
TTY: 301-468-5981
http://www.ninds.nih.gov/
American Academy of Neurology (AAN)
1080 Montreal Ave.
St. Paul, MN 55116
Phone: 651-695-2717
Toll-Free: 1-800-879-1960
Fax: 651-695-2791
http://www.thebrainmatters.org/
American Academy of Pediatrics (AAP)
141 Northwest Point Blvd.
Elk Grove Village, IL 60007-1098
Phone: 847-434-4000
Fax: 847-434-8000
http://www.aap.org/
Epilepsy Foundation of America (EFA)
8301 Professional Place
Landover, MD 20785
Toll-Free: 1-800-332-1000
http://www.epilepsyfoundation.org/