Peanut allergy effectively treated with oral immunotherapy: the PALISADE trial
1. After 24 weeks of oral immunotherapy treatment, patients with peanut allergy were able to consume significantly more peanut protein without allergic symptoms compared to patients treated with a placebo.
2. Treatment was shown efficacious is patients aged 4 to 17 and not efficacious in patients over 18 years of age.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Peanut allergy is prevalent in many industrialized countries and is becoming more common. This allergy can be life threatening and can persist throughout a patient’s lifetime. Current treatment options include avoidance, desensitization, and rescue medication utilization. A new orally available immunotherapy consisting of peanut protein, AR101, may provide a clinically useful method for treating patients with peanut allergy. The randomized Peanut Allergy Oral Immunotherapy Study of AR101 for Desensitization (PALISADE) trial evaluated patients with a low-threshold sensitivity to peanut protein and tested them again after 24 weeks of treatment with a higher peanut protein dose. For patients aged 4 to 17, those treated had significantly fewer allergic responses compared to those treated with placebo at the end of the trial. Therapy was not shown to be effective for patients over 18 years of age.
Strengths of this study include its randomized controlled design and its evaluation of a first-in-class treatment. Limitations include its limited inclusion of patients over 18 years of age and lack of statistical comparison of adverse events between the treatment and placebo groups.
Click to read the study, published today in NEJM
Relevant Reading: Effect of avoidance on peanut allergy after early peanut consumption
In-Depth [randomized controlled trial]: This multicenter, international, randomized controlled trial enrolled patients aged 4 to 55 who had a history of peanut allergy and positive peanut specific IgE levels. All patients had allergic reactions to a screening dose of 100 mg peanut protein. Patients were randomized in a 3:1 manner to receive AR101, a peanut-based biologic, or a placebo. Doses of treatment were escalated initially, then patients received 24 weeks of a maintenance phase consisting of 300 mg AR101 or a matching placebo. Following the maintenance phase, an exit-food challenge consisted of 300, 600, and 1000 mg peanut protein (as tolerated) to assess for peanut protein allergic response. A total of 551 patients received AR101 or placebo, and 55 patients were 18 years or older. Most patients had a history of asthma, peanut anaphylaxis, or multiple food allergies. At initial screening, the median tolerated dose of peanut protein was 10 mg. Of patients aged 4 to 17, 67.2% (250/372) of the treated patients were able to ingest 600 mg of peanut protein without dose-limiting symptoms at the exit-challenge compared to 4.0% (5/124) of those in the placebo group (between group difference of 63.2 percentage points; 95% confidence interval [CI], 53.0 to 73.3; P<0.001). Patients tolerated 1000 mg of peanut protein at rates of 50.3% vs 2.4% in the treatment and placebo groups, respectively. Severe allergic symptoms were elicited in 5% and 11% of the treatment and placebo groups, respectively, during the exit challenge (P<0.001). For patients aged 18 or older 41.5% and 14.3% of treatment and placebo patients tolerated 600 mg of peanut protein, which was not statistically significant. During the study, not including the exit challenge, 4.3% and 0.8% of patients experienced severe allergic symptoms.
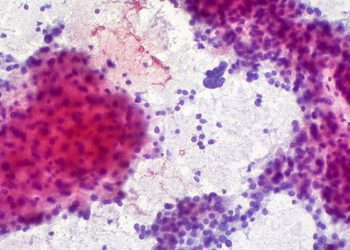
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-350x250.png)




