Robotic hysterectomy offers similar outcomes versus laparoscopic for benign disease
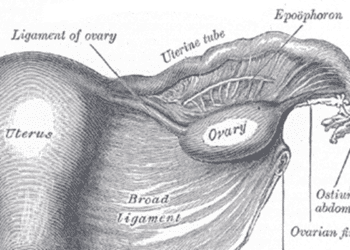
Image: PD
1. Robotic hysterectomies for benign gynecologic disease were not associated with improved overall outcomes compared to conventional laparoscopic hysterectomies.
2. Robotic hysterectomies for benign gynecologic disease were $2500 more expensive than laparoscopic surgeries.
Evidence Rating Level: 2 (Good)
Study Rundown: This retrospective cohort study found that though the use of robotics in minimally invasive surgery has increased significantly, robotic surgeries were not associated with improvement in overall outcomes compared with traditional laparoscopy.
This is one of the first nationwide studies to look at perioperative outcomes following benign hysterectomy by surgery type. Large sample size, nationally representative cohort and controlling for socioeconomic status and comorbidities are major strengths. Limitations include a higher prevalence of obesity and congestive heart failure in the robotic surgery group, which may bias results toward the null. The present work also did not account for level of training, familiarity with robotics or long-term outcomes. Future studies might stratify by patient BMI, surgeon’s level of training or number of robotic procedures performed and might include long-term follow-up, including a clinical indicator of adhesive disease.
Click to read the study in Obstetrics & Gynecology
Relevant Reading: Uptodate: Overview of hysterectomy
Study Author, Dr. Kimberly Kho, MD, MPH, talks to 2 Minute Medicine: University of Texas Southwestern Medical Center, Assistant Professor, Obstetrics & Gynecology
“From 2009 – 2010, though the use of robotic-assistance increased there was no improvement in perioperative outcomes compared to the laparoscopic approach and costs were significantly higher. Comparative effectiveness studies should encourage all of us in healthcare to critically appraise new technologies and find evidence to develop guidance for their appropriate use.”
In-Depth [retrospective study]: This study included women from a nationwide insurance database undergoing minimally invasive benign hysterectomy from 2009-2010 via robotic-assisted hysterectomy (n=7,788) and conventional laparoscopy (n=7,788). Primary outcome was a composite of in-hospital death and perioperative adverse events; secondary outcome was cost of hospital service. P value of <0.005 was considered statistically significant.
The use of robotic hysterectomy increased from 9.5% to 13.6% from 2009 to 2010 (p=.002). Overall complication rates were comparable between robotic and conventional laparoscopy (8.80% vs. 8.85%, p=.910). Compared with laparoscopic hysterectomies, robotic surgeries were less likely to require blood transfusion (RR=0.67, p<.001) but more likely to develop post operative pneumonia (RR=2.2, p=.005). Average in-hospital cost of robotic surgery was $2,489 (95% CI $2,313-2,664) more expensive than for laparoscopic surgery.
By Maren Shapiro and Leah Hawkins, MD, MPH
More from this author: IUD contraception equally safe in teenagers as in older women, Black men less likely to receive follow-up for elevated prostate cancer marker, PSA, Intake of fish fatty acids associated with lower risk of breast cancer, USPSTF recommends chemoprevention for women at high risk for breast cancer, Insurance status affects treatment of early stage breast cancer, SERMs decrease breast cancer risk even after treatment
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.