Some components of ventilator bundles may not improve patient outcomes
1. Based on this retrospective cohort analysis, most of the commonly used ventilator-bundles, including head-of-bed elevation, sedative infusion interruptions, spontaneous breathing trials, and thromboprophylaxis were all associated with decreased time to extubation. In addition, sedative infusion breaks and spontaneous breathing trials were associated with lower ventilator mortality.
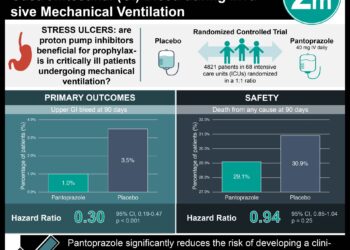
2. Oral care with chlorhexidine was associated with an increased risk of ventilator mortality. Stress ulcer prophylaxis was associated with increased risk for ventilator-associated pneumonia.
Evidence Rating Level: 2 (Good)
Study Rundown: Ventilator bundles include components such as head-of-bed elevation, sedative infusion breaks, spontaneous breathing trials, stress ulcer and thrombo- prophylaxis and oral care with chlorhexidine gluconate. These bundles have been created with the hopes of improving patient outcomes in intensive care units, however the benefits are unclear. This retrospective cohort study aimed to evaluate the associations between ventilator bundle components with overall outcomes amongst ventilated patients.
Individual ventilator bundle components varied in their association with patient outcomes. Head-of-bed elevation, sedative infusion interruptions, spontaneous breathing trials, and thromboembolism prophylaxis were associated with decreased time to extubation. Other positive correlations included lower hazard for ventilator mortality with sedative infusion interruptions and use of spontaneous breathing trials. However, oral care with chlorhexidine was associated with increase risk for ventilator mortality, and stress ulcer prophylaxis was associated with increased risk of ventilator-associated pneumonia. Strengths of the study included broad inclusion criteria (all ventilated patients over a particular time). The major limitation of this study was the observational design, wherein differences present in outcomes may have been from inherent differences in the cohorts rather than a direct relationship from the interventions.
Click to read the study, published today JAMA Internal Medicine
Relevant Reading: Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: Systematic review and meta-analysis
In-Depth [retrospective cohort study]: This study took place between January 2009 to December 2013 at Brigham and Women’s Hospital and included all 5,539 consecutive patients who underwent mechanical ventilation for a duration of at least 3 days. The exposures of interest included the different components of ventilator bundles: head-of-bed elevation, sedative infusion interruptions, spontaneous breathing trials, thromboprophylaxis, stress ulcer prophylaxis, and oral care with chlorhexidine. Outcomes of interest included ventilator-associated events, extubation alive versus ventilator mortality, and hospital discharge versus hospital death. Statistical analysis was done using Cox proportional hazards and Fine-Gray risk models adjusted for patient demographics, comorbidities, severity of illness, recent procedures, calendar year.
The mean age of the patients was 61.2 years. Exposures statistically associated with decreased time to extubation included sedative infusion interruption (HR 1.81; 95%CI 1.54-2.12), spontaneous breathing trials (HR 2.48; 95%CI 2.23-2.76), head-of-bed elevation (HR 1.38; 95%CI 1.14-1.68) and thromboembolic prophylaxis (HR 2.57; 95%CI 1.80-3.66). Decreased hazards for ventilatory mortality included sedative infusion interruptions (HR 0.51; 95%CI 0.38-0.68) and spontaneous breathing trials (HR 0.28; 95%CI 0.20-0.38). Oral care with chlorhexidine was associated with increase risk of ventilator mortality (HR 1.63; 95%CI 1.15-2.31) and stress ulcer prophylaxis was associated with increased risk of ventilator-associated pneumonia (HR 7.69; 95%CI 1.44-41.10).
Image: CC/Wiki
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.





![Adverse pregnancy outcomes associated with thrombophilias [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2015/07/Classics-2-Minute-Medicine-e1436017941513-75x75.png)