Symptoms of posttraumatic stress disorder highly prevalent among family members of patients admitted to the intensive care unit with COVID-19
1. Compared to prepandemic populations, family members of patients admitted to the intensive care unit with COVID-19 had significant symptoms of posttraumatic stress disorder 3 months after the patients’ admission.
2. Hispanic ethnicity, female gender, and previous medication use for a psychiatric condition were significantly associated with a higher degree of posttraumatic stress disorder symptoms.
Evidence Rating Level: 2 (Good)
Study Rundown: Symptoms of posttraumatic stress disorder (PTSD) in family members of patients admitted to the intensive care unit (ICU) have been well-described. However, it is uncertain how these psychological symptoms in family members have trended since the COVID-19 pandemic. This cohort study examined the potential consequences of pandemic-related restrictions and stress for families of critically ill patients with COVID-19, examining factors associated with stress-related symptoms. The main outcome was symptoms of PTSD at 3 months, defined by a score of ≥10 on the Impact of Events Scale 6 (IES-6). Among 330 family members of patients admitted to the ICU with COVID-19, family members experienced significant PTSD symptoms 3 months after the patients’ ICU admission. Hispanic ethnicity, female gender, and previous medication use for a psychiatric condition were significantly associated with a higher degree of posttraumatic stress disorder symptoms. Families with higher PTSD scores often experienced feelings of distrust towards healthcare practitioners due to pandemic restrictions and reduced interactions with the healthcare team. A limitation of this study was that due to the questionnaires being administered at 3 months after admission, there is a potential risk for recall bias among family members.
Click to read the study in JAMA Internal Medicine
Relevant Reading: A randomized trial of a family-support intervention in intensive care units
In-Depth [prospective cohort]: This cohort study included 330 family members of patients admitted to the ICU (mean [SD] age, 51.2 [15.1] years; 228 [69.1%] women; 150 [52.8%] White; 92 [29.8%] Hispanic) between February to July 2020 at 8 academic and 4 community hospitals in the US. Most participants were the patients’ child (129 [40.6%]) or partner (81 [25.5%]). At 3 months, the mean (SD) IES-6 score was 11.9 (6.1), with 63.6% of individuals with scores ≥10, indicating significant symptoms of PTSD. Compared to males, females had a higher adjusted mean score of 2.6 points (95%CI, 1.4-3.8; P < .001). Compared to non-Hispanics, Hispanic participants scored a mean of 2.7 points higher (95%CI, 1.0-4.3; P = .002). Compared to family members with a high school degree or equivalent, graduate school experience was associated with a lower adjusted mean score of 3.3 points (95%CI, 1.5-5.1; P < .001). Compared to family members with lower PTSD scores, those with higher scores demonstrated greater distrust of healthcare practitioners with no substantive differences in emotional or communication-related experiences.
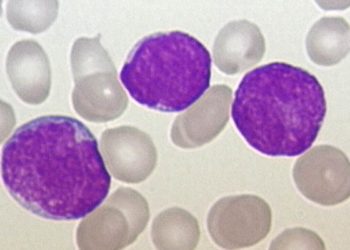
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.