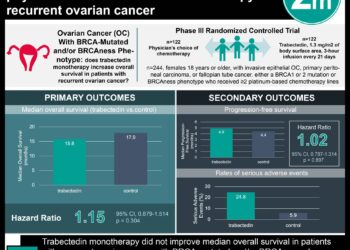
The LION trial: systemic lymphadenectomy in advanced ovarian cancer patients provides no survival benefits
1. Pelvic and paraaortic lymphadenectomy in advanced ovarian cancer patients provided no overall or progression-free survival benefits compared to patients not undergoing lymphadenectomy.
2. Serious postoperative complications, including postoperative death, occurred at greater rates in patients undergoing systematic lymphadenectomy.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Patients with advanced ovarian cancer generally receive surgery to remove all macroscopically visible tumor followed by chemotherapy. Some studies have suggested systematic pelvic and paraaortic lymphadenectomy provides additional survival benefit in these patients. The Lymphadenectomy in Ovarian Neoplasms (LION) trial sought to evaluate the survival benefit of systematic lymphadenectomy in patients with gross resection of advanced ovarian neoplasm. The median overall and progression-free survival rates did not differ between the groups receiving and not receiving lymphadenectomy, and patients undergoing lymphadenectomy experienced significantly greater postoperative complication rates.
This study provides compelling evidence that after complete macroscopic tumor resection, further lymphadenectomy in advanced ovarian cancer patients is unnecessarily morbid and provides no survival advantage. A limitation of this trial is generalizability as patients were treated at specialized surgical centers.
Click to read the study in NEJM
Click to read an accompanying editorial in NEJM
In-Depth [randomized controlled trial]: This multicenter randomized controlled trial enrolled patients between 2008 and 2012. Eligible patients had histologically proven stage IIB to IV epithelial ovarian cancer, had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, and macroscopic tumor resection appeared clinically feasible. Patients were randomized in a 1:1 ratio to undergo lymphadenectomy (n=323) or not (n=324), stratified by surgical center, age, and performance status. All operating surgeons were evaluated to have adequate surgical volume and performance prior to taking part in the study. The primary outcome of overall survival was 65.5 and 69.2 months in the lymphadenectomy and no-lymphadenectomy groups, respectively (hazard ratio for death in the lymphadenectomy group [HR], 1.06; 95% confidence interval [CI], 0.83 to 1.34; P=0.65). Progression-free survival also did not differ between groups, with a median of 25.5 measure in both (HR, 1.11; 95% CI, 0.92 to 1.34; P=0.29). Median duration of surgery was approx. 60 minutes longer in the lymphadenectomy group (P<0.001) and blood loss was also higher. More patients in the lymphadenectomy group required transfusions, had infections requiring treatment with antibiotics, and required postoperative admission to an intermediate care unit or ICU. Mortality at 60-days postoperatively was 3.1% (10/323] vs. 0.9% (3/324) in the lymphadenectomy and no-lymphadenectomy groups, respectively (P=0.049).
Image: PD
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc