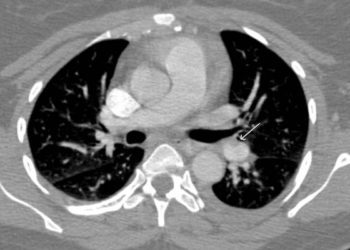
Vena cava filters plus anticoagulation do not prevent recurrent pulmonary embolism over anticoagulation alone
1. Placement of an inferior vena cava filter plus anticoagulation in high-risk hospitalized patients with acute pulmonary embolism did not prevent recurrence at either 3 or 6 months versus patients receiving anticoagulation alone.
Evidence Rating: 2 (Good)
Study Rundown: Prior studies have suggested recurrent pulmonary embolism (PE) may be reduced in patients with proximal deep vein thrombosis (DVT) who received full dose anticoagulation and inferior vena cava (IVC) filter placement as compared to those who received anticoagulation alone. These studies were performed before the implementation of modern anticoagulation strategies and widespread use of retrievable IVC filters, which subsequently reduced the risk of recurrent DVT secondary to filter thrombosis from permanently placed devices. Given these recent therapeutic evolutions, the current study sought to determine if temporary filter placement conferred a benefit to patients at risk of early PE recurrence.
In this randomized, open-label, blinded end point trial, hospitalized patients with acute PE were randomized to anticoagulation plus retrievable IVC filter placement or anticoagulation alone for prevention of recurrent PE, with filter removal set at 3 months. No difference in the rate of recurrent pulmonary embolism was detected between the groups at either 3 or 6 months, and no clinically significant filter thromboses occurred. Additionally, there was no difference in the rates of recurrent deep vein thrombosis, venous thromboembolism, major bleeding, or death within 6 months. Despite being one of the largest multi-center randomized trials using modern anticoagulation techniques and retrievable IVC filters, the study was limited by a lack of statistical power, as evidenced by the relatively wide confidence intervals when comparing the rates of recurrent symptomatic PE at 3 months. Additional limitations included heterogeneity in the types of anticoagulation employed, and a lack of inclusion of subjects who presumably would benefit most from IVC filter placement, such as critically ill patients or patients with unstable thrombus burden. Overall, this trial suggests that hospitalized patients with symptomatic PE arising from the lower-limbs do not benefit from the addition of IVC filter placement in addition to full-dose anticoagulation.
Click to read the study in JAMA
Relevant reading: Inferior vena caval filters: review of a 26 year single center clinical experience
In-Depth [randomized controlled trial]: In this randomized, open-label, blinded end point trial, a total of 399 high risk, hospitalized patients with acute pulmonary embolism and confirmed lower-limb venous thrombosis were randomized to anticoagulation and retrievable IVC filter insertion (n = 200) or anticoagulation alone (n = 199) and followed for six months after initiation of therapy. Those who had received IVC filters underwent device removal after three months, and all patients were fully anticoagulated for at least 6 months with either low molecular weight heparin, unfractionated heparin, fondaparinux, or a vitamin K antagonist. At three months, 3.0% of patients in the filter group experienced recurrent pulmonary embolism versus 1.5% in the control group (P = 0.50) constituting an insignificant difference. Placement of an IVC filter conferred a relative risk of 2.00 in the filter group with a markedly wide confidence interval (95% CI, 0.51-7.89), and no difference in the rates of recurrent PE after removal at 6 months. Additionally, there was no difference in the rates of recurrent deep vein thrombosis, venous thromboembolism, major bleeding, or death at 3 or 6 months between groups.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.