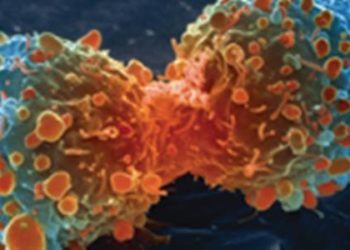
#VisualAbstract: Cemiplimab monotherapy significantly improves outcomes in patients with advanced non-small-cell lung cancer with PD-L1 of at least 50%
1. Median overall survival and progression-free survival were significantly improved with cemiplimab monotherapy compared to chemotherapy.
2. Patients treated with cemiplimab monotherapy reported fewer grade 3-4 adverse events.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Among patients with advanced non-small-cell lung cancer (NSCLC), a large proportion test positive for programmed cell death ligand 1 (PD-L1) in at least 50% of tumour cells. Currently, only one anti-PD-L1 therapy has been approved for use by the Food and Drug Administration. Cemiplimab is a highly potent monoclonal antibody that may be used for NSCLC, although limited research exists regarding its safety and efficacy. This randomized controlled trial compared the survival benefits of cemiplimab monotherapy with platinum-doublet chemotherapy in the treatment of advanced NSCLC with PD-L1 of at least 50%. Primary endpoints for this study were overall survival and progression-free survival, while secondary endpoints included objective response rate, duration of response, and health-related quality of life. According to study results, cemiplimab monotherapy resulted in a greater overall survival and progression-free survival, with fewer grade 3-4 treatment-related adverse events compared to chemotherapy. This study was strengthened by a variability in patient demographics (patients were selected from 24 countries) and longitudinal follow-up design (patients were assessed for up to two years from baseline). It provides valuable insight into the use of cemiplimab as a first-line monotherapy for patients with NSCLC and PD-L1 of at least 50%.
Click to read the study in The Lancet
Relevant Reading: PD-1 Blockade with Cemiplimab in Advanced Cutaneous Squamous-Cell Carcinoma
In-depth [randomized controlled trial]: Between Jun 27, 2017, and Feb 27, 2020, 710 patients were enrolled across 188 sites in 24 countries. Included patients were those ≥ 18 years old with histologically confirmed advanced NSCLC with PD-L1 ≥ 50% and Eastern Cooperative Oncology Group (ECOG) performance status of 0-1. Those who had never smoked and had tumours with EGFR mutations, ALK translocations, or ROS1 fusions were excluded. Altogether, 563 patients (283 in the cemiplimab group and 280 in the chemotherapy group) were include in analysis.
In the PD-L1 ≥ 50% population, median overall survival was not reached with cemiplimab (95% confidence interval [CI] 17.9-not evaluable) compared to 14.2 months (95% CI 11.2-17.5) with chemotherapy (hazard ratio [HR] 0.57, 95% CI 0.42-0.77, p=0.0002). The estimated probability of overall survival from baseline through 24 months was greater for cemiplimab (50%, 95% CI 36-63) versus chemotherapy (27%, 95% CI 14-43). This was also true for the primary outcome concerning median progression-free survival (8.2 months, 95% CI 6.1-8.8 with cemiplimab vs. 5.7 months, 95% CI 4.5-6.2 with chemotherapy, HR 0.54 [95% CI 0.43-0.68], p<0.0001). In the intention-to-treat population, significant improvement in overall survival and progression-free survival was reported with cemiplimab. Fewer grade 3-4 treatment-emergent adverse events occurred in the cemiplimab group (28%, 98 of 355 patients) compared to chemotherapy (39%, 135 of 342 patients). Overall, findings from this study support the use of cemiplimab monotherapy as first-line treatment in patients with advanced NSCLC with PD-L1 of at least 50%.
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![Fluorophores enhance visualization for image-guided surgery [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2015/01/FISH_13_21-350x250.jpg)