2 Minute Medicine Rewind February 19, 2018
Immunogenicity of Fractional-Dose Vaccine during a Yellow Fever Outbreak
There is currently a shortage of yellow fever vaccines in the face of outbreaks. In 2016, as it was proposed that a fractional dose of vaccine could also be protective, the Democratic Republic of Congo (DRC) held a large-scale vaccination campaign using a fractional dose of 17DD vaccine, constituting one-fifth of normal dose. In this prospective cohort study, investigators analyzed serum samples from 716 participants of this campaign in order to study the effect of fractional-dose vaccination on the generation of neutralizing antibodies against yellow fever virus. Participants who presented at one of six vaccination sites were approached for potential inclusion in the study, with an equal number of participants from four age strata: 2 to 5 years, 6 to 12 years, 13 to 49 years, and 50 years or older. Researchers found that out of the 493 (69%) of participants who were seronegative for neutralizing antibodies at baseline, 98% of these participants demonstrated evidence of seroconversion (95% CI 96% to 99%). Among participants, the lowest seroconversion rate was observed in children age 2 to 5 years, although between-group differences were not significant (p=0.06). In addition, seronegative males were more likely to have seroconversion than seronegative females (p=0.03). For participants already seropositive for yellow fever at baseline, 66% developed an immune response titer of >4 times the baseline value (95% CI 60% to 72%). An inverse correlation was observed between a participant’s baseline titer and likelihood of having an immune response (p<0.001). Overall, the results from this study indicate that a fractional dose of the current 17DD vaccine may be effective in inducing seroconversion and generation of an immune response. These findings support the use of fractional-dose vaccination for outbreak control.
Systolic Blood Pressure and Outcomes in Patients With Heart Failure With Preserved Ejection Fraction
The optimal systolic blood pressure (SBP) target for patients with heart failure (HF) with preserved ejection fraction (HFpEF) is not clear. In this retrospective cohort study, investigators analyzed data from a propensity score-matched patient cohort of 1802 hospitalized patients with HFpEF in order to examine the effect of having a SBP less than 120 mm Hg at discharge on 30-day, 1-year, and 6-year overall all-cause mortality and heart failure readmission. Researchers found that 30-day all-cause mortality occurred in 10% of patients with a discharge SBP <120 mm Hg and in 5% of patients with a discharge SBP >120 mm Hg (HR 2.07, 95% CI 1.45 to 2.95, p<0.001), All-cause mortality was also higher among individuals discharged with SBP <120 mm Hg at 1 year of follow-up (HR 1.36, 95% CI 1.16 to 1.59, p<0.001) and at 6 years of follow-up (HR 1.17, 95% CI 1.05 to 1.30, p=0.005). In terms of HF readmission, a SBP <120 mm Hg was associated with a higher risk at 30 days of follow-up (HR 1.47, 95% CI 1.08 to 2.01, p=0.02). Finally, patients discharged with SBP <120 mm Hg were found to be at an increased risk of experiencing the combined endpoint of heart failure readmission and all-cause mortality at 30 days (HR 1.71, 95% CI 1.34 to 2.18, p<0.001), 1 year (HR 1.21, 95% CI 1.07 to 1.38, p=0.004), and 6 years (HR 1.12, 95% CI 1.01 to 1.24, p=0.03) of follow-up. This study therefore shows that among hospitalized patients with HFpEF, SBP <120 mm Hg at discharge is associated with poorer outcomes. This study was limited in that there was no data on post-discharge SBP, and therefore SBP changes could have affected results. This study was also observational, and as such, future studies are needed in prospectively examining the effect of SBP treatment goals.
Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism
Current guidelines recommend a 6-month course of low molecular weight heparin (LMWH) as treatment for venous thromboembolism (VTE), a common complication of cancer and cancer therapy. This treatment, however, has imperfect compliance due to burdensome daily subcutaneous injections. Direct oral anticoagulant agents are as effective as vitamin K antagonists in the treatment of VTE, and are associated with less frequent and less severe bleeding. However, the use of these agents as compared to LMWH in the setting of cancer-associated VTE, has not yet been established. In this randomized controlled trial, 1050 cancer patients with acute or incidental VTE were randomized to receive either a course of subcutaneous LMWH (dalteparin 200 IU/kg) or a course of 5-day LMWH followed by oral edoxaban 60 mg once daily. Treatment was administered for at least 6 months and up to 12 months. The primary outcome studied was a composite of recurrent VTE or major bleeding during the 12 months after randomization, regardless of treatment duration. Researchers found that recurrent VTE or major bleeding occurred in 12.8% of participants in the edoxaban group and in 13.5% of participants in the dalteparin group (HR 0.97, 95% CI 0.70 to 1.36, p=0.006 for non-inferiority, p=0.87 for superiority). Subgroup analyses revealed that patients with gastrointestinal cancer were more likely to have an increased risk of bleeding with edoxaban compared to dalteparin (p=0.02). Taken together, the results of this study support that once-daily oral edoxaban is a non-inferior treatment compared to subcutaneous dalteparin for VTE, although it may increase the risk of major bleeding in gastrointestinal cancer patients. This study is limited in that it included patients with cancer who had received a wide variety of cytotoxic and biologic therapies. Further research is needed to predict the safety and efficacy edoxaban in different patient subgroups.
Real-time continuous glucose monitoring (rtCGM) has been proposed as a way to help optimize glycemic control in individuals with type 1 diabetes. However, there is little evidence available regarding the benefits of rtCGM for patients with problematic hypoglycemia. In this randomized controlled trial, 149 participants were randomly assigned to either rtCGM or to continue self-monitoring of blood glucose in order to determine whether the incidence and severity of hypoglycemia can be reduced through the use of rtCGM in high-risk individuals with type 1 diabetes. More than 90% of participants in this study had impaired hypoglycemia awareness. Researchers found that the mean number of hypoglycemic events per 28 days was reduced from 10.8 (SD 10.0) to 3.5 (SD 4.7) in the rtCGM group, and from 14.4 (SD 10.0) to 13.7 (SD 11.6) in the control group. The incidence of hypoglycemic events was also reduced by 72% for the rtCGM group (RR 0.28, 95% CI 0.20 to 0.39, p<0.0001). In comparison to the control group, the rtCGM group had a significantly reduced number of nocturnal hypoglycemic events (p<0.0001). In terms of serious adverse events, 7 occurred in the control group and 10 in the rtCGM group, although no event was considered related to the investigational device. Taken together, the results from this study support the use of rtCGM for patients with problematic hypoglycemia. The study is limited in that this was not a double-blind study, and participants were required to wear the rtCGM device 85% of the time, which may represent a source of selection bias and limit the generalizability of these findings to all high-risk individuals with type 1 diabetes.
Most research on single parenthood and its association with adverse health outcomes, including mortality, has focused on single mothers. The effect of single parenthood for single fathers, however, has not been well-studied. In this retrospective cohort study, investigators analyzed data on 871 single fathers, 4,590 single mothers, 16,341 partnered fathers, and 18,688 partnered mothers in examine the effect of being a single father on mortality in comparison to the other groups. Each group was followed up for a maximum of 15 years. Researchers found that in terms of mortality per 1000 person-years, partnered mothers had a mortality of 1.19 (95% CI 0.97 to 1.44), single mothers had a mortality of 1.74 (95% CI 1.23 to 2.41), partnered fathers had a mortality of 1.94 (95% CI 1.67 to 2.26), and single fathers had the highest mortality at 5.81 (95% CI 3.21 to 8.99). After adjustment for age and other factors, results showed that single fathers had twice the risk of mortality in comparison to single mothers (HR 2.49, 95% CI 1.20 to 5.15, p=0.01) and partnered fathers (HR 2.06, 95% CI 1.11 to 3.83, p=0.02). Results overall suggest that single fathers are at higher risk for premature mortality, which has implications for how healthcare systems should interact and support these individuals. This study is, however, limited in that it used the current marital status of individuals and did not look at the length of time individuals were single or partnered. Furthermore, the study used self-reported data to ascertain information on health behaviors. Future research should be conducted to better investigate risk factors that affect single fathers and understand potential causal pathways between single fatherhood and death.
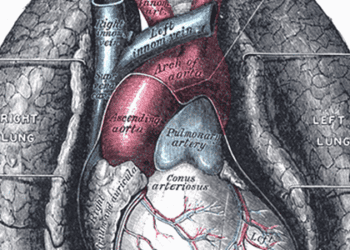
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.