2 Minute Medicine Rewind July 18, 2022
Association Between Time to Source Control in Sepsis and 90-Day Mortality
1. In a cohort of patients with sepsis, source control within 6 hours of sepsis onset was associated with a reduction in risk-adjusted odds of 90-day mortality compared with delayed source control.
Evidence Rating Level: 2 (Good)
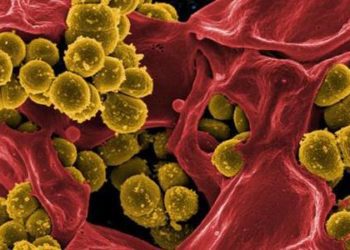
Sepsis is a condition associated with significant mortality. Source control is known to be a key step in early sepsis management. However, there is controversial data surrounding how rapidly source control should be achieved in a septic patient. Therefore, this cohort study sought to determine the association between the timing of source control and adjusted mortality in community-acquired sepsis. It made use of electronic health record data from a multihospital system. A total of 4962 (mean [SD] age, 62 [16] years; 52% male; 85% White; mean [SD] Sequential Organ Failure Assessment score, 3.8 [2.5]) patients with sepsis were included in the study. The study found that source control occurred at a median (IQR) of 15.4 hours (5.5 – 21.7) after sepsis onset and 1312 (27%) patients underwent source control within 6 hours. The primary outcome measured was 90-day postintervention mortality. It was found that early source control was associated with decreased risk-adjusted odds of 90-day mortality (aOR, 0.71; 95% CI, 0.63-0.80). The secondary outcomes measured included postintervention intensive care unit admission, hospital length of stay and in-hospital as well as 365-day mortality. The study found that source control was also associated with reduced risk-adjusted odds of in-hospital mortality (aOR, 0.76; 95% CI, 0.63-0.90; P = .002) and 365-day mortality (aOR, 0.66; 95% CI, 0.61-0.71; P < .001). Overall, the study concluded that source control within 6 hours of sepsis onset was associated with reduced risk of mortality.
1. In a cohort of patients undergoing laparoscopic surgery, total intravenous anesthesia maintained with remimazolam provides better quality of recovery than anesthesia maintained with an inhalant agent.
Evidence Rating Level: 1 (Excellent)
Quality of recovery post-operatively is highly associated with patient satisfaction and overall healthcare quality. Previous studies have demonstrated that total intravenous anesthesia (TIVA) promotes better quality of recovery than conventional anesthesia maintained by inhaled agents. Remimazolam is a novel intravenous benzodiazepine that is appropriate for maintenance of anesthesia. However, there is little published data on this drug. Therefore, this randomized-control trial compared the quality of recovery in patients undergoing TIVA with remimazolam versus balanced anesthesia. It included 168 patients, of which 82 (mean [SD] age, 43.4 (10.4); 20 male) were assigned to the intervention group and 83 (mean [SD] age, 43.2 (9.0); 18 male) were assigned to the control group. The intervention group received remimazolam at 1-2 mg/kg/hour while the control group was administered 0.7-0.9 MAC of desflurane. All other factors between the two groups remained the same, including the induction agents and the analgesia. The primary outcome measured was the perioperative decrement of the Quality of Recovery (QoR)-40 score, measured by subtracting the postoperative score from the preoperative score. The study found that the decrement of the QoR-40 score was smaller in the intervention group compared to the control group (26.99 versus 32.90, respectively; mean difference 5.91; 95% confidence interval, -0.96–12.79). After adjustment for factors such as age, type of surgery, and surgical time, the use of remimazolam was associated with a 7.03-point (95% CI 0.35–13.72) less decrement of the QoR-40 score than desflurane. Overall, the study concluded that TIVA with remimazolam provides a better quality of recovery than anesthesia maintained with an inhalant agent. However, additional randomized-control trials are needed to confirm and validate these results.
1. In a cohort of patients, isolated distal deep vein thrombosis was associated with lower risk of adverse events compared with a proximal deep vein thrombosis.
Evidence Rating Level: 2 (Good)
Deep vein thrombosis (DVT) can be associated with significant morbidity and mortality. Isolated distal deep vein thrombosis (IIDVT) account for about 20% – 50% of all DVTs. Some studies suggest better outcomes for patients with IDDVT. However, it is unclear whether there is a true difference between the two. Therefore, this multi-center cohort study aimed to address this gap by determining the clinical characteristics, short-term and 1-year outcomes in patients with IDDVT compared to those with a proximal DVT. It made use of data from the Registro Informatizado Enfermedad Tromboembólica (RIETE), an ongoing registry of patients with venous thromboembolism (VTE). 33 891 patients were identified with DVTs, of which 5938 (17.5%) had IDDVT (mean [SD] age, 61 [17] years; 2975 male patients [50.1%]), and 27 959 (82.5%) had proximal DVT (mean [SD] age, 65 [18] years; 14 315 male patients [51.2%]). The primary outcomes measured were 90-day and 1-year mortality, 1-year major bleeding, and 1-year VTE deterioration (defined as subsequent development of proximal DVT or PE). It was found that compared with individuals with proximal DVT, those with IDDVT has a lower risk of 90-day mortality (odds ratio [OR], 0.47; 95% CI, 0.40-0.55). The study demonstrated similar findings for 1-year mortality (hazard ratio [HR], 0.52; 95% CI, 0.46-0.59). It also found that patients with IDDVT had a lower 1-year risk of VTE deterioration (HR, 0.83; 95% CI, 0.69-0.99). Overall, the study concluded that IDDVT had a less ominous prognosis compared to proximal DVT. Future studies should further elucidate management strategies of IDDVT compared to proximal DVTs.
1. In a cohort of patients undergoing breast surgery, erector spinae plane block improved the quality of recovery compared to the control.
Evidence Rating Level: 1 (Excellent)
Regional anesthesia techniques are commonly used for breast surgery. The erector spinae plane block is a newer technique for delivering regional anesthesia to patients undergoing breast surgery. It has proven to reduce pain severity and opioid consumptions. However, there is a lack of data with regards to the quality of recovery in patients following this procedure. Therefore, this randomized control trial aimed to evaluate the quality of recovery in patients undergoing breast surgery receiving the procedure. It analyzed data from 65 patients who were randomized into either the control group (n=22), the sham block group (n=21) or the erector spinae plane (ESP) group (n=22). All patients were anesthetized in the same manner. Patients in the ESP group received a block at the level of T2 using 0.375% solution of ropivacaine at 0.4 mL/kg. Patients in the sham group were injected with 0.4 mL/kg of normal saline. The control group did not receive any further intervention beyond the general anesthesia. The primary outcome measured was the assessment of the patient’s improvement with quality of recovery (QoR)-40 a day after surgery. The study found that patients in the ESP group had improved QoR-40 compared to the control group (mean [interquartile range], 186 [177–193] vs. 175 [165–183]). The secondary outcomes measured were postoperative pain evaluation on the visual analog scale, 24-hour opioid consumption, time to the first opioid demand, and global satisfaction with preoperative treatment. It was found that acute postoperative pain severity was higher in the control group compared to the ESP group at postoperative hour 2 (p=0.012) and 4 (p<0.01). The study also found that postoperative oxycodone consumption was significantly higher in the control group compared to the ESP group. Patient satisfaction was also found to be higher in the ESP group compared to the control group. Finally, it was found that patients in the ESP group required their first dose of opioids significantly later compared to participants in the control group (3.65 [1.18–8.93] vs. 0.98 [0.61–2.81] hour; p = 0.014). Overall, the study concluded that The ESP block is superior to the control in terms of quality of recovery in patients undergoing breast surgery. However, additional randomized control trials with larger sample sizes are needed to further validate the results of this study.
Preclinical Aortic Atherosclerosis in Adolescents With Chronic Disease
1. In a large cohort of adolescents, chronic disease was found to be associated with enhanced aortic stiffness and wall thickness compare to controls.
Evidence Rating Level: 2 (Good)
Adolescents with chronic disease are known to be exposed to long term inflammatory abnormalities which can accelerate atherogenesis. Studies have found that adolescents with chronic disorders are known to have an enhanced cardiovascular risk. Nonetheless, it is challenging to detect early atherosclerosis in adolescents. Therefore, there is limited research in this field. As a result, this study aimed to investigate preclinical atherosclerosis in adolescence with chronic diseases using aortic measures. It enrolled 114 adolescents 12 to 18 years old with disorders such as juvenile idiopathic arthritis (n=20), cystic fibrosis (n=24), obesity (n=20), and corrected coarctation of the aorta (n=25). Health adolescents with a corrected atrial septal defect were used as controls (n=25). The study utilized cardiovascular magnetic resonance to assess aortic pulse wave velocity and aortic wall thickness. These are established aortic measures of preclinical atherosclerosis, which was the primary outcome measured in the study. It was found that adolescence in all chronic disease groups demonstrated increased aortic stiffness and higher aortic wall thickness compared with controls (p<0.05). The study concluded that the enhanced aortic pulse wave velocity and aortic wall thickness in patients with chronic disease could indicate accelerated atherogenesis. However, future studies with a larger sample size and long-term follow-up are needed To validate these results.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.