2 Minute Medicine Rewind June 9 – June 15, 2014
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
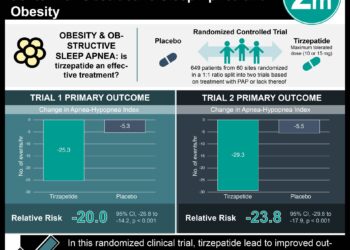
CPAP, Weight Loss, or Both for Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) and obesity are both independently associated with insulin resistance, dyslipidemia, hypertension, and inflammation. They are also strongly associated to each other. In this randomized controlled trial, 181 patients with obesity, moderate-to-severe OSA, and serum levels of C-reactive protein (CRP) greater than 1.0 mg/L were randomized to continuous positive airway pressure (CPAP), a weight-loss intervention, or CPAP plus a weight-loss intervention for 24 weeks. CRP levels, insulin resistance, dyslipidemia, and blood pressure were significantly reduced in the weight loss only group but not in the CPAP only group. Although the combined intervention provided no significant incremental effect on CRP levels, it provided greater reduction of insulin resistance, blood pressure and serum triglyceride levels compared with either weight loss or CPAP alone. Thus, in patients with moderate-to-severe sleep apnea and obesity, the addition of weight loss in addition to CPAP may improve cardiovascular outcomes.
Transoral Robotic Surgery for Obstructive Sleep Apnea in Asian Patients
The 15-year mortality for adults with severe obstructive sleep apnea (OSA), when left untreated, is increased by 30%. The standard OSA treatment is continuous positive airway pressure (CPAP); however, surgery is available for those who cannot tolerate CPAP. Transoral robotic surgery (TORS) for tongue base reduction and partial epiglottidectomy has been shown to be safe and efficient in Europe and in the United States. However, OSA is known to be far more severe when adjusted for sex, age, and BMI in Asian patients compared with other ethnic groups, likely because of contribution from skeletal structural restriction. In this retrospective study, data from 20 Asian patients with moderate to severe OSA who underwent primary TORS tongue base reduction with partial epiglottidectomy and palatal surgery after failed CPAP treatment were analyzed. Post-operatively, 7 (35%) had an apnea-hypopnea index [AHI] <5/h (traditional cure), 11 (55%) had an AHI <20 (>50% reduction in AHI – traditional success) and 2 (10%) failed to show clear improvements. The mean (SD) Epworth Sleepiness Scale score and snoring loudness on the visual analog scale were both significantly improved, from 12.4 (2.87) to 6.4 (1.43) and 8.7 (0.8) to 3.5 (1.7), respectively (P < .001 for both). No hypoglossal nerve injury, or lingual artery injury were recorded; tonsillar fossa bleeding, pain, temporary dysgeusia, numbness of the tongue, and temporary dysphagia were noted. This study showed that TORS tongue base reduction and partial epiglottidectomy is safe and effective for Asian patients with moderate to severe OSA who have failed CPAP treatment.
Brodalumab, an Anti-IL17RA Monoclonal Antibody, in Psoriatic Arthritis
Tumor necrosis factor (TNF) inhibitors have shown great therapeutic benefits for patients with psoriatic arthritis, a chronic inflammatory disorder associated with substantial disability and reduced life expectancy; however, many continue to have poor disease control, generating a need for new kinds of treatment. Brodalumab, a human monoclonal antibody against interleukin-17 receptor A (IL17RA), has shown 75% improvement in the psoriasis area-and-severity index (PASI) score in early studies. In this Phase 2 randomized controlled trial, 168 patient with active psoriatic arthritis were randomized to receive brodalumab (140 or 280 mg subcutaneously) or placebo on day 1 and at weeks 1, 2, 4, 6, 8, and 10. At week 12, higher rates of American College of Rheumatology response criteria (ACR 20) were since in the brodalumab 140-mg groups (37% [P=0.03]) and 280-mg (39% [P=0.02]), compared to the placebo group (18%). Responses were sustained through week 52. Serious events occurred in 3% of patients in the brodalumab groups and in 2% of those in the placebo group. Although longer studies are needed, this study demonstrates the safety and efficacy of brodalumab for patients with active psoriatic arthritis.
Hydrolyzed Infant Formula and Early β-Cell Autoimmunity
Recent studies suggest that exposure to complex foreign proteins in early infancy may increase the risk of β-cell autoimmunity and type 1 diabetes in genetically susceptible individuals. Feeding at risk children with extensively hydrolyzed formula, which do not contain intact proteins, therefore has the potential to decrease the cumulative incidence of diabetes-associated autoantibodies in young children. In this randomized clinical trial, 2159 infants with HLA-conferred disease susceptibility and a first-degree relative with type 1 diabetes were randomized to extensively hydrolyzed casein formula or a conventional cows’ milk–based formula. Autoantibodies to insulin, glutamic acid decarboxylase, and the insulinoma-associated–2 (IA-2) molecule all predict clinical type 1 diabetes. Positivity for at least 2 autoantibodies signals a risk of approximately 60% for the development of clinical diabetes over 10 years. The absolute risk of positivity for 2 or more islet autoantibodies was 13.4% for infants in the casein hydrolysate formula group compared to 11.4% for those in the conventional formula group. The rate of complications was not significantly different between the two groups. Thus, no benefit can currently be reported from using hydrolyzed formula in infants at risk for Type I diabetes.
The Swedish Obese Subjects (SOS) study demonstrated that bariatric surgery reduces the long-term incidence of diabetes by about 80%. However, little is known about the long-term health effects of this diabetes remission. In this study, patients from the SOS prospective matched cohort study with baseline type II diabetes (343 of 2010 surgery patients and 260 of 2037 control patients) were followed for 15 years. Two year after surgery, patients in the bariatric surgery group (adjustable or nonadjustable banding (n = 61), vertical banded gastroplasty (n = 227), or gastric bypass (n = 55)) had a diabetes remission rate of 72.3% (95% CI, 66.9%-77.2%; 219/303) compared to 16.4% (95% CI, 11.7%-22.2%; 34/207) for patients in the control group (odds ratio [OR], 13.3; 95% CI, 8.5-20.7; P < .001). Fifteen years after surgery, patients in the bariatric surgery group had a diabetes remission rate of 30.4% compared to 6.5% for patients in the control group (OR, 6.3; 95% CI, 2.1-18.9; P < .001). The cumulative incidence of microvascular complications was 20.6 per 1000 person-years (95% CI, 17.0-24.9) in the surgery group and 41.8 per 1000 person-years (95% CI, 35.3-49.5) for control patients (hazard ratio [HR], 0.44; 95% CI, 0.34-0.56; P < .001). Although these results should be verified in randomized trial, this long-term observational study demonstrates that the benefits of bariatric surgery continue to exist more than a decade after surgery.
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.