2 Minute Medicine Rewind October 20, 2025
Glucose-Lowering Medication Classes and Cardiovascular Outcomes in Patients With Type 2 Diabetes
1. In patients with type 2 diabetes (T2D), the risk of major adverse cardiovascular events (MACEs) was lowest among patients undergoing sustained treatment with glucagon-like-peptide-1 receptor agonists (GLP-1RAs), followed by sodium-glucose cotransporter-2 inhibitors (SGLT2is), sulfonylureas and dipeptidyl peptidase-4 inhibitors (DPP4is).
Evidence Rating Level: 2 (Good)
MACEs remain the leading cause of mortality in patients with T2D. Previous studies have shown that GLP-1RAs and SGLT2is significantly reduce the incidence of MACEs in adults living with T2D, yet few studies have compared the protective effects of the various antihyperglycemic agents used in the management of T2D in preventing MACEs. This retrospective cohort study therefore sought to compare the risk of MACEs in adults with T2D receiving four different antihyperglycemic agents for T2D. 241,981 adults (mean [SD] age, 57.2 [12.9] years; 54.3% male) with T2D from 6 health care delivery systems across the United States were included in this study. Patients in this study were separated into groups based on medication classes (GLP-1RAs, SGLT2is, sulfonylureas and DPP4is). When comparing the cumulative incidence across the four groups, the adjusted 2.5 year average risk difference (ARD) showed a decrease in MACE risk over time with GLP-1RAs compared with SGLT2is (ARD, −0.006 [95% CI, −0.008 to −0.004]; P < .001), sulfonylureas (ARD, −0.013 [95% CI, −0.015 to −0.012]; P < .001), and DPP4is (ARD, −0.015 [95% CI, −0.018 to −0.011]; P < .001). Similarly, there was a decrease in MACE risk over time with SGLT2is compared with sulfonylureas (ARD, −0.007 [95% CI, −0.009 to −0.005]; P < .001) and DPP4is (ARD, −0.009 [95% CI, −0.013 to −0.005]; P < .001). Lastly, there was a decrease in MACE risk over time with sulfonylureas compared with DPP4is (ARD, −0.001 [95% CI, −0.005 to 0.002]; P = .47). Overall, this study found that among adult patients with T2D in the United States, GLP-1RAs offered the greatest protective effect against MACEs, followed by SGLT2is, sulfonylureas and DPP4is.
Smartphone-Based Muscle Relaxation for Migraine in the Emergency Department
1. Among adults presenting to the emergency department (ED) with migraine, a smartphone-based progressive muscle relaxation (PMR) program significantly reduced migraine-related disability compared with usual care.
Evidence Rating Level: 1 (Excellent)
Migraine is a common cause of ED visits, but over half of these patients do not have a prior migraine diagnosis and preventive management is rarely initiated at discharge. This 2-group parallel-group randomized control trial evaluated whether a smartphone-based app (RELAXaHEAD) could improve patient-reported migraine outcomes. 94 patients (median age 33 years, 82.6% female) were randomized in a 1:1 fashion to use RELAXaHEAD as a symptom-reporting diary and PMR management vs. as a symptom-reporting diary alone. Patients in the PMR group completed a 5-minute deep-breathing session, a 6-minute PMR session (brief), a 12.5-minute PMR session (full), and an 8.5-minute muscle scan session for a minimum of 60 days during the 90-day treatment period. Patients using PMR had a significantly greater reduction in migraine-related disability (mean change −25.1 vs +6.9; p = 0.01), as measured by the migraine disability assessment. No significant differences were seen in migraine-specific quality of life (MSQv2 questionnaire) or monthly headache days. Overall, app-based PMR reduced migraine-related disability following ED discharge and represents a feasible, low-cost behavioral intervention for migraine management.
1. In patients with previously treated extensive-stage small-cell lung cancer (ES-SCLC), treatment with ifinatam deruxtecan (I-DXd) showed promising efficacy with an objective response rate (ORR) of 48.2% and a 9-month overall survival (OS) estimate of 59.1%.
Evidence Rating Level: 1 (Excellent)
Patients with ES-SCLC currently have a very poor prognosis, with a lack of an accepted standard-of-care therapy after first-line chemoimmunotherapy. I-DXd is a novel antibody-drug conjugate which has shown promising efficacy in patients with previously treated SCLC in the phase 1 IDeate-PanTumour01 trial. The IDeate-Lung01 trial is therefore a phase 2 trial designed to investigate the efficacy and safety of I-DXd in patients with previously treated ES-SCLC. Between May 2022 and June 2024, 183 patients over the age of 18 with ES-SCLC previously treated with between 1 and 3 lines of systemic therapy were included in the study, with 88 patients enrolled in the dose optimization portion of the study and 95 enrolled in the extension portion of the study. In patients receiving the highest dose (12-mg/kg group), the confirmed ORR was 48.2% (95% CI, 39.6-56.9%) with a progression-free survival at 6 and 9 months of 35.3% (95% CI, 27.3-43.4%) and 19.3% (95% CI, 12.9-26.5%), respectively. The median OS was 10.3 months (95% CI, 9.1-13.3%). Among the 12-mg/kg group, treatment-emergent adverse events (TEAEs) were reported in 39.4% (54/137) of patients, with TEAEs associated with death being reported in 6 patients. Overall, this phase 2 study found that in patients with ES-SCLC, treatment with I-DXd showed promising efficacy with a manageable safety profile.
1. Among patients with adult-onset inflammatory bowel disease (IBD), the incidence of ocular manifestations was 2.9 per 1000 person-years.
2. The incidence of ocular manifestations was higher in patients with Crohn’s disease (CD) than ulcerative colitis (UC).
Evidence Rating Level: 2 (Good)
Extraintestinal manifestations are common in patients with IBD, with ocular manifestations such as episcleritis and scleritis representing the third most commonly affected organ system. Previous studies have reported that the prevalence of ocular manifestations in IBD may range from 2 to 12%, yet longitudinal data remain limited, especially in the adult IBD population. This retrospective cohort study therefore sought to investigate the incidence of ocular manifestations in patients with adult-onset IBD. 15,035 patients (median age at diagnosis[IQR], 37.4[26.3-52.1] years; 51.8% CD; 50.72% female) with new-onset IBD between 2005 and 2024 from the Maccabi Healthcare Services in Israel were included in this study. The incidence of ocular manifestations was 2.9 per 1000 person-years (95% CI, 2.62-3.24%) with a cumulative incidence of 1.7%, 2.7% and 3.7% at 5, 10 and 15 years, respectively. Among patients who developed an ocular manifestation, 63.3% (221/349) of patients had CD while 36.6% (128/349) had UC. Overall, this study found that the incidence of ocular manifestations in patients with adult-onset IBD was 2.9 per 1000 person-years and higher among patients with CD compared with UC.
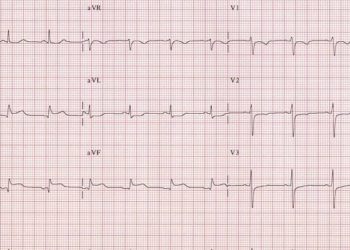
1. At one month, ticagrelor was not superior to twice-daily clopidogrel in reducing major adverse cardiovascular events (MACEs) in adult patients receiving primary percutaneous coronary intervention for ST-segment elevation myocardial infarction (STEMI).
Evidence Rating Level: 1 (Excellent)
The highest risk period for MACEs after primary PCI for STEMI is in the first month. Both ticagrelor and double-dose clopidogrel have been shown to improve patient outcomes after acute coronary syndrome. However, no study has compared these strategies in the early high-risk post-STEMI period. This double-blind, randomized controlled trial analyzed whether ticagrelor is superior to twice-daily clopidogrel in reducing 30-day MACEs in adult patients with STEMI undergoing primary PCI. 2,201 patients (mean[SD] age, 54.8 ± 10.1 years; 87.3% male) to receive either clopidogrel 75 mg twice daily or ticagrelor 90 mg twice daily for one month. All patients received aspirin 75 mg daily. At 7 and 14 days, there was a significantly lower incidence of MACEs in patients receiving ticagrelor ((HR: 0.15; 95% CI: 0.04-0.5; P = 0.002) and (HR: 0.46; 95% CI: 0.23-0.91; P = 0.02), respectively), although these differences were no longer statistically significant at 30 days (HR: 0.75; 95% CI: 0.44-1.27; P = 0.28; absolute risk difference: -0.7%; 95% CI: -2.05 to 0.60). The ticagrelor group had a higher risk of any bleeding event (HR: 2.08; 95% CI: 1.10-3.93), as defined by the Bleeding Academic Research Consortium (BARC) criteria, but there was no significant difference in the incidence of clinically significant or major bleeding (BARC 2, 3, 5; HR: 1.50; 95% CI: 0.42-5.31). Overall, ticagrelor was not superior to twice-daily clopidogrel in reducing MACEs at 1 month after primary PCI. However, further studies with larger cohorts are warranted as MACEs were significantly reduced in patients receiving ticagrelor at 7 and 14 days.
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.