Alzheimer disease diagnoses aided by amyloid positive PET scans
1. A meta-analysis of amyloid-b-specific positron emission tomography studies in patients with dementia suggests that amyloid positivity decreases with age in patients with Alzheimer type dementia, while it increases in most non-Alzheimer type dementias.
2. Carriers of apolipoprotein E ε4 had higher mean prevalence of amyloid positivity than noncarriers making diagnoses based on amyloid positivity less reliable in this subgroup.
Evidence Rating Level: 1 (Excellent)
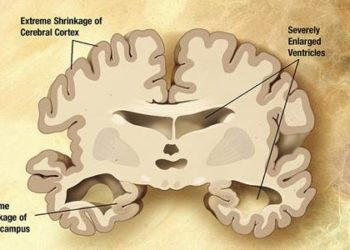
Study Rundown: Alzheimer disease (AD) is the most common cause of dementia and its earliest recognizable pathological event is cerebral amyloid-b aggregation. While many factors contributing to dementia in AD have been studied, the mainstay of diagnosis remains clinical examination. Additional techniques including genetic analysis and amyloid-specific positron emission tomography (PET) scans are valuable diagnostic adjuncts with currently unclear utility. Further investigation into the prevalence of amyloid pathology is needed in patients with varying forms of dementia to allow for better interpretation of amyloid-positive imaging studies used in the quantification of cerebral amyloid deposition. Given that amyloid is also known to deposit in healthy patients without cognitive symptoms, the association between amyloid positivity and age, sex, education level, and global cognitive ability must be understood to better support detection and early treatment.
The current study sought to estimate the prevalence of amyloid positivity on amyloid-specific PET scans across multiple dementia types through a meta-analysis of roughly 30 cohorts. The analysis revealed that the prevalence of amyloid positivity increased with age in patients with non-AD dementias, while it decreased with age in those with AD and corticobasal-type dementias. Among carriers of the Apolipoprotein E (APOE)-ε4 gene, amyloid positivity was significantly more prevalent, and increased at an accelerated rate with age. Independently, amyloid positivity was also associated with worse global cognitive function. Given these patterns of prevalence between the various forms of dementia, amyloid PET scans may be valuable in development of a differential diagnosis in early-onset dementias or as a confirmatory study in patients over age 70 years. The study was limited in terms of generalizability as most subjects were highly educated, no racial or ethnic data was included, and there were small numbers of patients over age 80 years. Additional biases may be present due to the heterogeneity of study designs included, and due to a lack of pathologic data to confirm dementia subtype in all patients. Future studies are necessary to better understand the role of amyloid PET imaging in dementia diagnostics, with particular regard to the elderly, specific racial or ethnic groups, and in light of differences in accuracy between various PET tracers.
Click to read the study in JAMA
Relevant Reading: Apolipoprotein E polymorphism and Alzheimer disease.
In-Depth [meta-analysis]: A total of 1897 patients with dementia (mean age 65.9 to 74.5, depending on dementia type; 50.2% male) drawn from 29 previously published cohorts were included, which were matched to 1849 control subjects from 23 separate cohorts. Studies were included based on availability of participant-level data on amyloid status per an amyloid-specific PET study, age, sex, education level, APOE-ε4 status and clinical scores of cognition by either the Mini-Mental State Examination (MMSE) or the Clinical Dementia Rating. Of those patients with dementia, 1359 had AD, 288 had frontotemportal dementia, 138 had vascular dementia, 51 had dementia with Lewy bodies, and 61 had corticobasal syndrome. The prevalence of amyloid positivity was 88% overall in AD dementia, decreasing with age from 50 years (93%) to 90 years (79%) with an estimated prevalence of amyloid positivity per year of -0.032 (p < 0.001). Among APOE-ε4 carriers, prevalence was 90% regardless of age. In non-AD dementia, amyloid prevalence was highest in dementia with Lewy bodies, followed by vascular and frontotemporal dementias, with increasing amyloid prevalence with age at an estimated prevalence per year of 0.042 (p < 0.01). Amyloid positivity was associated with decreased global cognitive scores in both AD and non-AD dementias. In AD patients, mean MMSE scores for amyloid positive patients was 21.2 versus 22.2 for amyloid negative patients (p < 0.05), while the difference was even greater for non-AD patients with mean scores of 20.6 versus 23.2 (p < 0.001). Amyloid positivity prevalence was not significantly associated with either sex or years of education in either AD or non-AD dementias. The odds ratio for discrimination of AD from non-AD subjects based on amyloid PET imaging decreased in all non-AD dementias as age increased, except in those with corticobasal syndrome.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.