Brain metastases in germ cell tumors associated with poor prognosis
1. In a retrospective review of over 500 men with germ cell tumors, the presence of brain metastases (BM) was associated with poor overall survival.
2. Multimodal treatment with high-dose chemotherapy may improve survival among patients with germ cell tumors who relapse with brain metastases.
Evidence Rating Level: 3 (Average)
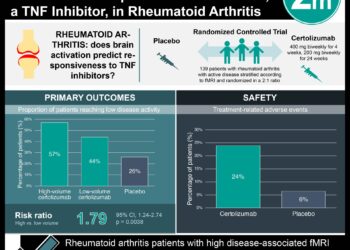
Study Rundown: Brain metastases (BM) from germ cell tumors (GCT) are rare, but are associated with overall poor prognosis. Men with GCT may present with BM at the time of diagnosis (synchronous) or at the time of disease relapse (metachronous). Given the low incidence of BM, the mainstay management for these two patient populations remains under debate, with strategies ranging from chemotherapy alone to multimodality treatment including surgery, radiotherapy, and chemotherapy. The purpose of this large, retrospective cohort study was to evaluate the treatments, outcomes, and prognostic factors in these two patient populations.
The study retrospective reviewed the survival data of over 500 men with BM secondary to GCT and categorized them as either synchronous or metachronous BM. At the conclusion of the study, both groups demonstrated poor overall survival (OS); however, patients presenting with synchronous disease demonstrated improved survival compared to the metachronous BM. Adverse prognostic factors for both groups included number of BM and the presence of liver or bone metastases. Additionally, multimodality treatment and high-dose chemotherapy were associate with improved overall survival in the metachronous BM group only. The results of this trial supports the use of multimodal treatment with high-dose chemotherapy in patients presenting with BM after GCT relapse. This trial was limited by the retrospective observational nature of the study and could not account for potential confounders and selection and reporting bias. However, this is the largest patient series to analyze the outcomes of this group of patients and provided important management and prognostic information for this patient population.
Click to read the study in JCO
In-Depth [retrospective cohort]: This cohort study included data from 523 patients with BM secondary to GCT from multiple centers in Canada, Australia, Europe, and United States. Patients were excluded if the BM diagnosis was post mortem or had been previously treated for any brain tumors. Patients were categorized based on whether BM was detected at the time of diagnosis (group A) or at the time of disease relapse (group B). The primary end point was overall survival (OS). End points were calculated from time of initiation of first line treatment (group A) or salvage therapy (group B). At the conclusion of the study, the median OS was significantly higher in group A compared to group B (29.6 months vs. 8 months; p<0.001). In group A, the presence of liver and/or bone metastases (HR: 2.11; 95% CI: 1.47 to 3.03; p<0.001), and the presence of multiple BM (HR: 1.88; 95% CI: 1.24 to 2.85; p=0.003) were associated with poor OS. In group B, multiple BM (HR: 2.00; 95% CI, 1.40 to 2.87; p<0.001), liver and/or bone metastases (HR: 1.92; 95% CI: 1.29 to 2.84; p<0.001), and elevated alpha-fetoprotein and/or HCG (HR: 2.11; 95% CI: 1.48 to 3.02; p<0.001) were associated with poor OS. In group A, there was no benefit with multimodality treatment (p = 0.07) or high-dose chemotherapy (p = 0.62) for OS after adjusting for prognostic factors. In group B, multimodality treatment (p < 0.001) and high-dose chemotherapy (p < 0.001) significantly improved OS.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.