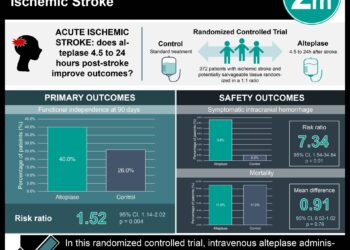
Early administration of thrombolytics in ischemic stroke associated with reduced all-cause mortality and readmissions
1. Patients who received tPA within 45 minutes of hospital arrival had a statistically significant reduction in all-cause mortality, all-cause readmission, and composite all-cause mortality or readmission than patients who received tPA after 45 minutes.
2. All-cause mortality at 1-year increased significantly for every 15-minute delay in tPA administration within 90 minutes of door-to-needle time.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Clinical data from the GWTG-Stroke database, consisting of patients who were older than 65 who received tPA after presenting to participating hospitals with acute ischemic stroke within 4.5 hours of symptom onset, was retrospectively analyzed. This study found that patients who received tPA after 45 minutes had a statistically significant increase in all-cause mortality and readmission rates, and cardiovascular readmission rates within one year, as compared to patients who received tPA in under 45 minutes. Patients who received tPA more than 60 minutes after hospital arrival also had significantly increased all-cause and composite mortality and readmission rates at one year, compared to patients who received it in under 60 minutes. Further, there was found to be a positive relationship between door-to-needle time and mortality and readmission rates, at each 15 minute interval, within 90 minutes of tPA administration. While further study is necessary, the results of this study indicate that a reduction in door-to-needle time may improve health outcomes and further reinforce the importance of timely tPA administration. This study was limited by lack of inclusion of patients under the age of 65 and non-medicare recipients. Further, the majority of hospitals participating in this database were academic or primary stroke centers, while only 3% of included patients were treated in rural hospitals.
Click to read the study, published today in JAMA
Relevant Reading: Use of Strategies to Improve Door-to-Needle Times With Tissue-Type Plasminogen Activator in Acute Ischemic Stroke in Clinical Practice
In-Depth [retrospective cohort]: Tissue plasminogen activator (tPA) thrombolytic therapy is widely used in the treatment of acute ischemic stroke. Faster door-to-needle time, as opposed to delayed treatment, has previously been shown to be associated with a decrease in adverse side effects (such as intracranial hemorrhage) and improvement in functional outcomes at 3 months. This study, as part of a quality improvement initiative, sought to further delineate the effect of door-to-tPA times on 1-year all-cause and composite mortality and readmission rates in patients with acute ischemic stroke.
Retrospective analysis of clinical data from the GWTG-Stroke database, collected from 2006-2016, was performed. Long-term outcomes were assessed using Medicare claims files. Of the 61,426 patients included in this study, all were Medicare recipients over the age of 65 (median age 80), 82% were non-Hispanic white, and 43.5% were male. All had known acute ischemic strokes and received tPA within 4.5 hours of the time that they were last known to be asymptomatic. Exclusion criteria included: patients who did not receive tPA, patients whose door-to-tPA time was not available, patients who received concomitant intra-arterial reperfusion therapy, and patients who were transferred out of the hospital or left AMA.
Outcome, mortality, and readmission data of patients who received tPA in under 30 minutes, 30-45 minutes, 45-60 minutes, and greater than 60 minutes of hospital arrival was analyzed and compared. Patients who received tPA more than 45 minutes after hospital arrival, as compared to those who received it within 45 minutes, had a statistically significant increase in all-cause mortality (35% vs 30.8%), all-cause readmission rates (40.8% vs 38%), and cardiovascular related readmission rates (19.8% vs 18.4%). Patients who received tPA more than 60 minutes after hospital arrival, as compared to within 60 minutes, also had a significant increase in all-cause mortality (35.8% vs 32.1%), all-cause readmission rates (41.3% vs 39.1%), composite all-cause mortality or readmission rates (56.8% vs 53.1%) and cardiovascular readmission rates (20.2% vs 18.6%). There was no significant change in these outcomes in patients who received tPA within 30 minutes of arrival versus after 30 minutes of arrival. Furthermore, all cause mortality was found to linearly and positively increase at each 15 minute timepoint within 90 minutes.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.