HPV vaccine effective against infection and for herd immunity
1. Human papillomavirus (HPV) vaccine decreased infection rates among vaccinated women by 70-80%, depending on vaccine type
2. Infection with 4-valent vaccine-type HPV among unvaccinated women also decreased by about 40%.
Study Rundown: Current literature suggests HPV infection is linked to several types of female and male genital, anal, and oropharyngeal cancers. Previous studies have demonstrated the efficacy of the 3 HPV vaccines licensed in the United States in reducing vaccine-type HPV in the community, however the impact on herd immunity is unclear. Researchers in this study analyzed genotype data on HPV infection in vaccinated and unvaccinated women during the 11-year period after the first vaccine was released in the US (2006 to 2017). They sought to evaluate the effectiveness and herd protection of the 4-valent and 9-valent HPV vaccines, which prevent 4 and 9 cancer-causing strains of HPV, respectively. Results showed that the odds of infection with 4-valent and 9-valent vaccine-type HPV at the end of the study period were about 1/10 and 1/5 times the odds of infection at the beginning of the study. While the odds of infection with 4-valent vaccine-type HPV among unvaccinated women decreased by 50% over the study period, the odds of infection with 9-valent vaccine-type HPV did not change significantly in this population. Vaccine rates increased by about 85%, and the study found overall 4-valent vaccine rates of >95% by the end of the study. This study is limited by the restricted geographical recruitment region and the small number of participants who received the 9-valent HPV vaccine. Nonetheless, these findings suggest the 4-valent vaccine is effective in reducing 4-valent vaccine-type HPV infection rates among vaccinated and unvaccinated women, and pediatricians should continue to educate patients on the benefits of these vaccinesContinued surveillance is required to study the longevity of vaccine effectiveness and effects of the 9-valent vaccine on infection rates.
Click to read the study, published today in Pediatrics
Recommended reading: HPV infection rates in men
In-depth [surveillance study]: In this study, researchers analyzed surveillance data collected from one major U.S. city during 4 one-year waves between 2006 and 2017 to determine the proportion of vaccinated and unvaccinated women aged 13 to 26 years (N=1580, 72.8% African American/multiracial, 26.8% white) who were vaccine-type HPV positive (4-valent, 9-valent, or 5 additional strains not covered by the 9-valent vaccine). Results showed 80.6% participants reported ≥2 male sexual partners in their lifetime, and 16.9% reported their age of first sexual encounter to be ≤13 years. Rates of HPV vaccination (receipt of ≥ 1 dose with either vaccine) rose consistently between each wave, from 0% during the 1st wave to 84.3% in wave 4. By the end of the study, 97% of participants had received the 4-valent vaccine. The odds of infection with 4-valent and 9-valent vaccine-type HPV decreased significantly among vaccinated women (adjusted odds ratio [aOR] 0.13 and 0.18, respectively) between wave 1 and wave 4. The odds of infection with 4-valent vaccine-type HPV decreased significantly among unvaccinated women (aOR 0.50) but infection with 9-valent vaccine-type HPV did not change significantly. The odds of infection with ≥1 of the 5 additional HPV types in the 9-valent vaccine decreased significantly among vaccinated women (aOR 0.26) but increased significantly among unvaccinated women (aOR 1.90) between wave 1 and wave 4.
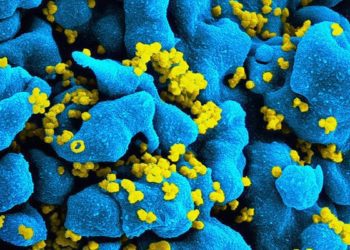
Image: PD
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.