Intensified treatment does not improve outcomes in tuberculous meningitis
1. Intensified antituberculosis treatment was not associated with a higher rate of survival among patients with tuberculous (TB) meningitis than standard treatment.
2. This study does not support a change in the current recommended treatment regimens for TB meningitis.
Evidence Rating Level: 1 (Excellent)
Study Rundown: TB meningitis kills or disables roughly half of patients with the condition, despite early anti-TB chemotherapy therapy and adjunctive glucocorticoids. Current guidelines for TB meningitis are based on data from pulmonary TB and do not sufficiently consider the ability of these drugs to enter the brain. This study sought to test the hypothesis that higher dose rifampin and the addition of levofloxacin for the first eight weeks of treatment would show lower rates of death and disability from TB meningitis than in those who received the current standard of care.
All patients received standard, empiric, oral, anti-TB therapy: rifampin, isoniazid, pyrazinamide, and ethambutol for three months, followed by rifampin and isoniazid for an additional six months. All patients received adjunctive dexamethasone for the first six to eight weeks of treatment. The study group received intensified treatment with levofloxacin and an additional 5 mg/kg/day of rifampin. In HIV-infected patients, antiretroviral therapy that was started before enrollment was continued unless contraindicated for use with rifampin.
There was no statistically significant difference between the standard-treatment and intensified-treatment groups in the primary outcome. A significantly higher frequency of seizures and visual impairment was reported in the intensified group compared to the placebo group. This study draws strength from its prespecified calculation of the number of total patients, including a minimum of 350 HIV-infected patients, to have 80% power to detect a 10% lower 9-month risk of death between the groups and an approximately equal number of HIV-infected patients in each group. However, it is limited by its design which tested a regimen rather than the contributions of individual drugs.
Click to read the study, published today in NEJM
Relevant Reading: Tuberculous meningitis: more questions, still too few answers
In-Depth [randomized controlled trial]: This randomized, double-blind, placebo-controlled trial of adults with a clinical diagnosis of TB meningitis compared a standard 9-month regimen to an intensified regimen. 817 adult patients underwent randomization to receive either standard treatment plus either placebo (n=409) or additional rifampin or levofloxacin (n=408). The intensified regimen added rifampin (5 mg/kg/day) and levofloxacin (20 mg/kg/day) to the standard regimen. The standard regimen consisted of rifampin (10 mg/kg/day), isoniazid (5 mg/kg/day up to 300 mg/day), pyrazinamide (25 mg/kg/day up to 2 g/day), ethambutol (20 mg/kg/day up to 1.2 g/day) followed by rifampin and isoniazid at the same doses for an additional 6 months. For patients with rifampin and/or isoniazid resistant M. tuberculosis, treatment was adjusted in accordance with local practices and susceptibility of the organism.
The primary outcome of the study was death by 9 months after randomization. The secondary outcomes were neurologic disability at 9 months, time to the first new neurologic event or death, and serious adverse effects. There was no evidence of a differential effect of intensified treatment on the primary outcome: 113 patients in the intensified-treatment and 114 patients in the standard-treatment group died (HR= 0.94; 95% [CI], 0.73 to 1.22; p = 0.66). The only statistically significant differences in secondary outcomes between the treatment groups were a higher frequency of seizures in the intensified-treatment group (23 vs. 11, p = 0.04) and a higher frequency of visual impairment in the intensified-treatment group (14 vs. 4, p = 0.02).
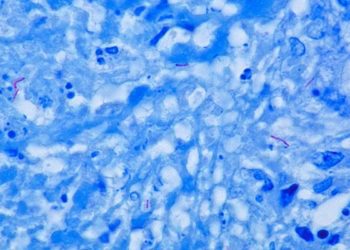
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.