No difference in safety or efficacy of low-dose alteplase for treatment of lacunar acute ischemic stroke
1. Patients with lacunar acute ischemic stroke treated with low-dose alteplase had a lower incidence of intracranial hemorrhage compared with those treated with standard-dose, but did not experience any benefit with regards to disability or death.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Patients presenting with acute ischemic strike (AIS) routinely receive intravenous thrombolysis. Though there is an inherent risk of intracranial hemorrhage (ICH) associated with the administration of thrombolytic agents, the benefits often outweigh the risks. However, there is some concern about the risks associated with thrombolysis among patients with lacunar AIS in particular, where the benefit of thrombolysis is more modest. The Enhanced Control of Hypertension and Thrombolysis Stroke Study (ENCHANTED) was a 2015 randomized trial showing that a lower dose of intravenous alteplase, a commonly used thrombolytic agent, had a lower risk of ICH compared with standard-dose alteplase among AIS patients. This is a post-hoc analysis of the ENCHANTED trial, with the primary research question being whether there is any difference in efficacy or safety between low- and standard-dose intravenous alteplase among participants with lacunar and non-lacunar AIS in the alteplase cohort of the ENCHANTED trial.
Patients included for this analysis were more likely to be older and have a higher baseline NIHSS score. Furthermore, patients with definite/probable lacunar AIS experienced better 90-day functional outcomes compared with patients with definite/probable non-lacunar AIS. They were also less likely to experience ICH or death after the administration of alteplase. With regards to the primary research question, among patients in the “definite” subgroup of lacunar AIS, there was no significant difference between the low- and standard-dose alteplase groups, nor was there a significant difference with regards to major disability or death. It should be noted, however, that only five participants experienced ICH between both the low- and standard-dose cohorts.
Strengths of this analysis include utilizing data from a large, prospective study with multiple adjustments made for covariables. Additionally, the reviewers of radiographic imaging were blind to clinical data and followed a rigorously designed approach. A limitation that should be noted is that the low incidence of ICH among patients with lacunar AIS limits the statistical conclusions that can be drawn from comparing the two doses. In all, however, this post-hoc analysis of the ENCHANTED trial found no clear evidence that low-dose alteplase is superior to standard-dose among patients with lacunar AIS, and thus these patients should receive standard-dose alteplase if eligible for thrombolysis.
Click here to read the study in Neurology
Relevant reading: Low-Dose versus Standard-Dose Intravenous Alteplase in Acute Ischemic Stroke
In-depth [post-hoc analysis]: 2,588 of the original 3,297 study participants were eligible for analysis; 195 with “definite lacunar” AIS, 295 with “probable lacunar” AIS, 1,697 with “definite non-lacunar” AIS, and 401 with “probable non-lacunar” AIS. Compatible with the findings of ENCHANTED, participants as a whole in this sub-group analysis had lower incidence of ICH if receiving low-dose alteplase, but there was no difference in effect on functional outcomes (modified Rankine scale [mRS] 2-6: aOR 1.04, 95% CI 0.87 to 1.24). This analysis found no differential treatment effects of low- compared with high-dose alteplase on all outcomes across lacunar and non-lacunar AIS (all p interactions ≥ 0.07). Moreover, in the “definite lacunar” AIS subgroup specifically, there was no significant difference between low-dose and standard-dose alteplase with regards to disability or death (mRS 2-6: 33.7% vs. 32.9%, aOR 0.96, 95% CI 0.49 to 1.87).
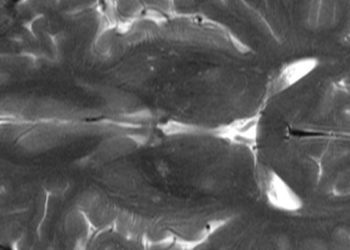
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.