Non-contrast CT sensitive and specific for kidney stones [Classics Series]
This study summary is an excerpt from the book 2 Minute Medicine’s The Classics in Medicine: Summaries of the Landmark Trials
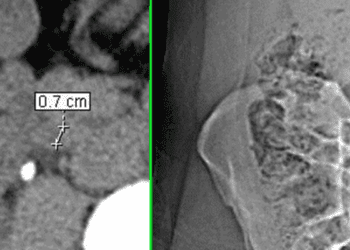
1. Among patients with acute flank pain, non-contrast computed tomography (CT) of the abdomen and pelvis demonstrated a sensitivity of 97% and a specificity of 96% for the diagnosis of kidney stones.
2. Non-contrast CT was associated with a low false negative rate and was able to suggest alternative diagnoses in a significant number of patients without evidence of kidney stones, thus increasing the overall diagnostic yield.
Original Date of Publication: January 1996
Study Rundown: Kidney stones, or nephrolithiasis, are a common cause of pain among patients presenting to the emergency department. Historically, the evaluation of patients with suspected nephrolithiasis consisted of plain radiographs together with clinical history, physical examination, and laboratory data. However, this combination was associated with a high false negative rate. The diagnostic yield was improved with the widespread adoption of intravenous pyelography (IP), a fluoroscopic technique in which dye is introduced into the urinary tract and imaged by x-rays in real-time. The use of IP improved stone detection but was associated with higher radiation exposure and the need for contrast administration, and the false negative rate remained high. There remained a significant need for a fast, accurate diagnostic technique among patients with suspected stone disease. With the introduction of CT into standard practice, there was a strong push towards its adoption as the standard for evaluation of nephrolithiasis given its high spatial and contrast resolution. In the present study, patients with symptoms concerning for nephrolithiasis were imaged with non-contrast CT of the abdomen and pelvis to determine the presence or absence of stones within the urinary tract. These patients then underwent a combination of repeat imaging, surgery, or close clinical follow-up to determine the final diagnosis. The results suggested that non-contrast CT was highly sensitive and specific for the nephrolithiasis, as well as associated with few false negative findings. Moreover, because of the ability to imaging other structures within the abdomen and pelvis in high resolution, CT was able to identify possible alternative diagnosis, such as appendicitis or infection, in nearly 33% of patients without evidence of stones. The study was limited by the use of a composite reference standard and the lack of outcome data. Today, non-contrast CT in conjunction with ultrasonography remains the diagnostic gold standard among patients with suspected kidney stones.
Click to read the study in the American Journal of Roentgenology
In-Depth [prospctive cohort]: A total of 292 consecutive patients referred for evaluation of possible nephrolithiasis at a single center underwent non-contrast CT of the abdomen and pelvis by standard protocol. Images were blindly reviewed by 2 radiologists with expertise in CT interpretation, and imaging diagnoses were made by consensus. Findings considered positive for nephrolithiasis included direct visualization of a stone within the ureters or bladder, or unilateral collecting system dilation and perinephric stranding without direct stone visualization. Of the original cohort that underwent imaging, 210 patients (98 male, 112 female; age range 18-85 years) went on to have diagnostic confirmation in the form of surgery, repeat imaging, or clinical follow-up. The results of the study suggested a sensitivity and negative predictive value of 97%, and a specificity and positive predictive value of 96%. The overall diagnostic accuracy of non-contrast CT in the evaluation of patients with suspected nephrolithiasis was 97%. Thirty-one patients without evidence of stone disease on CT (27.6%) were found to have unsuspected extra-renal abnormalities, the most common of which was symptomatic adnexal masses.
Smith RC, Verga M, McCarthy S, Rosenfield AT. Diagnosis of acute flank pain: value of unenhanced helical CT. American Journal of Roentgenology. 1996 Jan 1;166(1):97–101.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.