Patient Basics: Colonoscopy
Originally published by Harvard Health.
What Is It?
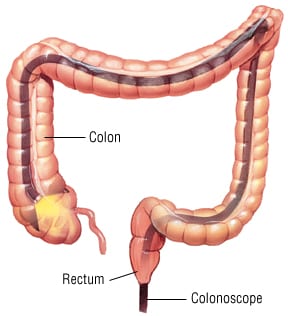
Colonoscopy is an examination of your complete colon, or large intestine. Colonoscopy is similar to another type of exam called sigmoidoscopy, which looks at only the last part of the colon. To perform colonoscopy, your doctor uses an instrument called a colonoscope, which is a flexible viewing tube with lenses, a small TV camera and a light on one end. Through bundles of flexible glass fibers (fiber-optic technology) and a small video computer chip, the colonoscope scans the inside of your colon and transmits images to a video screen.
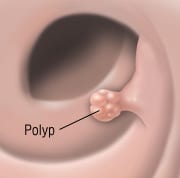
During colonoscopy, your doctor can check your colon for abnormal growths called polyps, sites of bleeding and for other conditions such as colitis. The procedure may take up to an hour and is done in a special endoscopy suite or the outpatient area of a hospital. Although the colonoscope is lubricated and bends easily, you will be lightly sedated to minimize any discomfort.
What It’s Used For
Colonoscopy is used to look at the lining of your colon. This makes it useful in detecting colon cancer, polyps, inflammation and other problems of the gastrointestinal tract. To screen routinely for colon cancer, your doctor may recommend colonoscopy every 7 to 10 years. Colonoscopy should begin earlier in people with a high risk of colorectal cancer due to a family history of colorectal cancer, chronic inflammatory bowel disease or certain hereditary syndromes, including familial adenomatous polyposis. Regular colonoscopy at more frequent intervals also is recommended for anyone who has already had either a cancerous growth or precancerous polyp removed from the bowel.
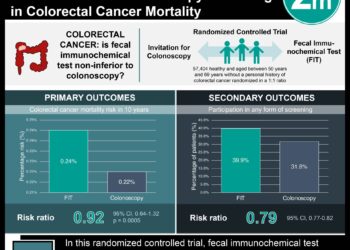
Colonoscopy may be done as a follow-up exam after a positive fecal occult blood test. It also can be used to identify the source of rectal bleeding or to confirm that there are areas of colitis (inflammation of the colon) in someone who has symptoms.
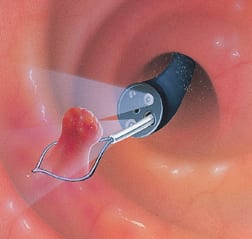
If your doctor sees a suspicious area during colonoscopy, he or she can use an attachment at the end of the colonoscope to take a biopsy (small tissue sample) to be examined in a laboratory. If a polyp is found during colonoscopy, your doctor may use a wire loop attachment to remove the entire polyp so that it can be sent for laboratory analysis.
Preparation
Your bowel needs to be empty during colonoscopy to give your doctor a clear view of your intestinal wall. To help empty your bowel, your doctor will give you specific directions about using laxatives the day before the procedure. Different doctors may recommend different laxative regimens, with or without enemas. In some cases, you will also need to follow a liquid diet for one to two days before the procedure with a full fast (nothing by mouth) after midnight the evening before the procedure. Your doctor will give you more exact details about diet when you schedule your colonoscopy exam. Because you will receive medication during colonoscopy that may make you feel drowsy, arrange for a friend or family member to help you get home from the doctor’s office.
How It’s Done
You will put on a hospital gown, and the doctor’s assistant will record your vital signs, including temperature, pulse and blood pressure. A pulse oximeter (to measure the oxygen saturation level of your blood) may be placed on your finger, ear or toe, and electrocardiograph (EKG) recording patches will be placed on your chest to monitor your heartbeat. You will be asked to lie on your side on an examination table, with the lower portion of your body covered by a sheet. As your doctor directs, you may be asked to raise one or both of your knees up to your chest. You will be given medication that will lightly sedate you and help your doctor insert a lubricated, flexible colonoscope into your rectum and, as necessary, pump a small amount of air through the colonoscope to open up your intestinal passage for a clearer view. Your doctor may also take a stool sample or biopsy from inside your bowel.
Follow-Up
After colonoscopy is done, you can get dressed. However, because you may still feel drowsy from the medication, a friend or family member should help you get home. You may pass gas that was pumped into your bowel during the examination.
You may return to your normal diet whenever you wish. If your doctor took a stool sample or biopsy during the exam, check back in a few days for the results.
Risks
In about 1 to 3 out of every 1,000 colonoscopies, a serious complication will occur. This can include heavy bleeding or a puncture or injury to the bowel wall.
When To Call a Professional
Call your doctor immediately if you see rectal bleeding after colonoscopy or if you feel faint, dizzy or short of breath or have palpitations. Also call your doctor if you have nausea, vomiting, cramps or any other type of abdominal pain or if you develop a fever, chills, severe headache or muscle aches.
Additional Info
American Cancer Society (ACS)
1599 Clifton Road, NE
Atlanta, GA 30329-4251
Toll-Free: 1-800-227-2345
http://www.cancer.org/
National Cancer Institute (NCI)
U.S. National Institutes of Health
Public Inquiries Office
Building 31, Room 10A03
31 Center Drive, MSC 8322
Bethesda, MD 20892-2580
Phone: 301-435-3848
Toll-Free: 1-800-422-6237
TTY: 1-800-332-8615
http://www.nci.nih.gov/

![2MM: AI Roundup- AI Cancer Test, Smarter Hospitals, Faster Drug Discovery, and Mental Health Tech [May 2nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/Untitled-design-350x250.png)