
Want more physician-written
medical news?
Join over 10 million yearly readers and numerous companies. For healthcare professionals
and the public.
Subscribe for free today!
Originally published by Harvard Health.
End-stage renal disease is a condition in which the kidneys no longer function normally. “Renal” describes anything having to do with the kidneys. Nearly everyone is born with two kidneys. They both need to fail for end-stage renal disease to develop.
Kidneys eliminate poisons from the body, and keep a normal balance of fluid and certain minerals in the body. When the kidneys can no longer perform this function, a person becomes very ill and ultimately dies.
In end-stage renal disease, the kidneys function at a fraction of their normal capacity. When this occurs, there are only two options: replace the job the kidneys are supposed to do by using a machine, instead (kidney dialysis) or transplant a new, healthy kidney. A single new kidney can do the work of the two kidneys.
Diabetes is the leading cause of end-stage renal disease. Kidney disease can result from type 1 or type 2 diabetes. With either type, poor control of blood sugar increases the risk of end-stage renal disease.
Other common causes of end-stage renal disease are:
Symptoms of end-stage renal disease include:
Symptoms may remain mild or absent until kidney function drops to less than 20% of normal.
Dialysis is urgent when one or more of the following occurs:
Dialysis may also be necessary if symptoms affect quality of life or nutritional status. This is especially true if they are accompanied by severely abnormal blood tests.
Kidney disease is diagnosed through urine and blood tests. These tests measure levels of creatinine and urea nitrogen in the urine and blood.
Additional tests may be necessary to determine why the kidneys have stopped working.
End-stage renal disease is a lifelong condition unless a kidney transplant is done. Even with a successful transplant, a person must take medicine for the rest of his or her life.
You can take steps to reduce your risk of developing end-stage renal disease:
The two treatments for end-stage renal disease are dialysis and kidney transplant.
Dialysis
There are two types of dialysis:
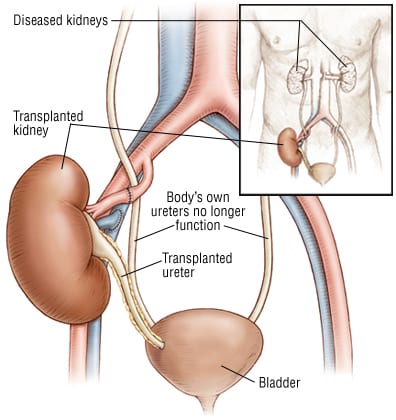
Kidney transplants
Kidney transplants allow people with severe kidney disease to avoid or discontinue dialysis. However, even a successful kidney transplant is not a cure.
Anyone who receives a kidney transplant must take immunosuppressive drugs for life, unless they received a kidney donated by their identical twin. These are drugs that prevent the body from rejecting the donated organ. In addition, a good genetic match is needed for a successful transplant. Most transplant candidates wait one to three years before they are matched to a kidney from an unrelated donor.
 |
You should have regular checkups if you have:
These checkups should include urine and blood tests to measure your kidney function.
When blood tests indicate kidney disease, your doctor should refer you to a kidney specialist. This specialist is called a nephrologist.
Call your doctor if you notice any decrease in urination or other symptoms of end-stage renal disease. Be particularly vigilant if you have kidney disease or its risk factors.
When kidney failure occurs, treatments offer hope for good recovery. Many people on dialysis or who have received transplants lead near normal lives.
National Institute of Diabetes & Digestive & Kidney Disorders
Office of Communications and Public Liaison
Building 31, Room 9A04
31 Center Drive, MSC 2560
Bethesda, MD 20892-2560
Phone: 301-496-4000
http://www.niddk.nih.gov/
National Kidney Foundation
30 East 33rd St.
New York, NY 10016
Phone: 212-889-2210
Toll-Free: 1-800-622-9010
Fax: 212-689-9261
http://www.kidney.org/
2 Minute Medicine is the leading authoritative medical news licensing service, and the only with reports written by practicing doctors.

No ads & unlimited access to all current reports, over 9000 searchable archived reports, visual abstracts, Weekly Rewinds, and the online edition of The Classics Series™ textbook.
2 Minute Medicine® is an award winning, physician-run, expert medical media company. Our content is curated, written and edited by practicing health professionals who have clinical and scientific expertise in their field of reporting. Our editorial management team is comprised of highly-trained MD physicians. Join numerous brands, companies, and hospitals who trust our licensed content.
© 2021 2 Minute Medicine, Inc. - Physician-written medical news.

Join over 10 million yearly readers and numerous companies. For healthcare professionals
and the public.
Subscribe for free today!