Prevalence of cerebral palsy in preterm infants changes over time
1. In preterm infants followed over a 3.75-year study period, the overall prevalence of cerebral palsy (CP) decreased from 16% to 12%, the prevalence of severe CP decreased from 26% to 16%, but the prevalence of mild CP increased from 39% to 43%
2. Overall rates of moderate to severe neurodevelopmental impairment (NDI) did not significantly change over time in this group of preterm infants.
Evidence Rating Level: 2 (Good)
Study Rundown: The National Institute of Child Health and Human Development’s (NICHD) Neonatal Research Network (NRN) has been publishing neurodevelopmental outcomes in premature infants since 1993. Studies evaluating neurodevelopmental outcomes in preterm infants over the past decade have focused primarily on moderate to severe impairment. In this retrospective cohort study, researchers aimed to describe a broader spectrum of neurodevelopmental outcomes, including milder forms of impairment. Specifically, they evaluated neurodevelopment via Bayley Scales of Infant Development (BSID-III), cerebral palsy diagnosis, sensory impairment and a composite NDI score. Their data showed that BSID-III cognitive scores did not vary significantly over the 3.75-year study period. BSID-III cognitive and motor scores tended to be worse the younger the gestational age (GA) of the subject. Both the prevalence of receiving a general CP diagnosis and the prevalence of severe CP decreased slightly over time. In contrast, the prevalence of mild CP increased. The prevalence of sensory impairment (specifically, hearing impairment and bilateral blindness) was rare. Composite NDI scores did not change significantly over time. Limitations of this study included lack of a term control group, a short study period of 3.75-years, and a group of subjects lost to follow-up (11%) who were significantly less likely to have late-onset sepsis, severe intraventricular hemorrhage, and fewer ventilator days. For pediatricians, this study highlights the changing developmental profile of preterm infants, which may allow for earlier identification of developmental delay and the need for interventional services in certain populations.
Click to read the study published today in Pediatrics
Click to read an accompanying editorial in Pediatrics
Relevant Reading: Trends in care practices, morbidity, and mortality of extremely preterm neonates
Study author, Ira Adams-Chapman, MD, MPH, talks to 2 Minute Medicine:
Emory University School of Medicine and Children’s Healthcare of Atlanta.
This article is an important read for providers caring for prematurely born children so that they have a full understanding of the neurodevelopmental outcomes of contemporary NICU graduates. The spectrum of outcome has shifted towards an increase in milder forms of motor delay and an increase in cognitive delay.
In-Depth [retrospective cohort]: The study was conducted across 21 NRN-affiliated centers over a 3.75-year period (April 1, 2011 to January 15, 2015). Participants included 2113 infants with a mean GA of 25±1.0 weeks and mean birth weight of 760±154 grams. Inclusion criteria was GA≤27 weeks, while exclusion criteria included chromosomal anomalies and/or major birth defects. Primary outcomes included BSID-III composite and subscale scores for cognitive and motor domains, cerebral palsy, sensory impairment, and a composite NDI score. For the overall BSID-III cognitive composite score, 10% and 28% of subjects had scores of <70 and <85, respectively, and these scores did not change significantly over time. The mean BSID-III cognitive score was 89.2±15.4 for all infants. The mean BSID-III composite motor score was 87.7±16.4 for all infants. The mean gross motor and fine motor scaled scores for all infants were 7.5±2.8 and 8.6±2.9, respectively, for all infants. In general, as subjects’ GA increased, BSID-III cognitive and composite motor scores increased.
Overall, a CP diagnosis was made in 12% of participants: 41% had mild CP, 40% had moderate CP, and 18% had severe CP. Moderate CP was defined as gross motor function classification system (GMFCS) level of 2-3, while severe CP was defined as GMFCS level of 4-5. Over the study period, the prevalence of CP decreased from 16% to 12% and the rate of severe CP decreased from 26% to 16%. However, the prevalence of mild CP increased from 39% to 43%. Regarding sensory impairment, 3% were diagnosed with hearing impairment and 1% were diagnosed with bilateral blindness. Moderate to severe NDI scores were defined by one or more of the following: BSID-III cognitive score <70 and motor score <70, a GMFCS level GMFCS level ≥2 (with or without moderate or severe CP), bilateral blindness and/or hearing impairment. In terms of NDI scores, the prevalence of individual components decreased over time, but only the aforementioned rates of CP differed significantly. The rate of severe NDI decreased over the study period when using both a BSID-III cognitive cutoff of <70 and <85, but these changes were not significant.
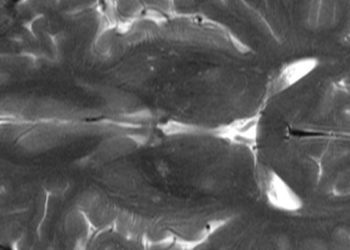
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.