Shorter time to angioplasty may improve heart attack outcomes
1. Patient mortality rates associated with primary percutaneous coronary intervention (pPCI) increased between 2005 and 2011, despite decreases in door-to-balloon (DTB) times.
2. Although mortality rates increased, the decrease in DTB times was associated with decreased mortality events, suggesting that the overall trend of increasing mortality is a consequence of changing treatment procedures and patient characteristics.
Evidence Rating Level: 2 (Good)
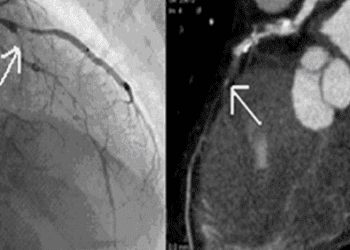
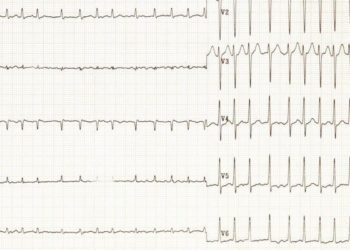
Study Rundown: Multiple studies have shown longer delays between myocardial infarction and angioplasty treatment, or pPCI, are associated with increased muscle death and worse patient outcomes. However, recent population studies have shown increased broad patient pPCI-associated mortality, despite decreasing DTB times. In this retrospective study of approximately 150 000 pPCI procedures, researchers found that mortality from 2005 to 2011 had increased despite a decrease in DTB times by approximately 27%. When researchers investigated the correlation of individual DTB times with individual patient outcomes, they found that longer DTB times were associated with greater mortality risk. Researchers postulate that the increase in patient mortality is a result of a changing patient population and changes in treatment protocols, and that work aimed to decrease DTB times is justified, and does improve patient outcomes.
While the findings of this retrospective study are purely correlative, they do provide important evidence that decreased DTB times are associated with decreased mortality risk. Future studies will be needed to shed further light on the reasons behind the increasing mortality rates of the pPCI patient group.
Click to read the study in The Lancet
Click to read an accompanying editorial in The Lancet
Relevant Reading: Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction
In-Depth [retrospective cohort]: This study examined data collected on 150 116 pPCI procedures performed between 2005 and 2011. Approximately, 25% of the procedures were performed in patients aged 65 years or older. The primary endpoints were in-hospital mortality, and 6-month mortality (only evaluated for patients aged 65 years or older). DTB times, defined as the time from hospital arrival to first device use during pPCI, were calculated for each patient and subsequently used to calculate a yearly median DTB. Collected patient characteristics data included patient sex, age, and gender, and treatment characteristics data included anticoagulant and stent type.
Between 2005 and 2011, risk-adjusted in-hospital mortality increased from 4.7% to 5.3% (p=0.06) and risk-adjusted 6-month mortality increased from 12.9% to 14.4% (p=0.001). The median patient DTB decreased from 86 minutes in 2005 to 63 minutes in 2011. Multiple other factors associated with the patient cohort and treatment protocol also varied over the 7-year period including rates of thrombin inhibitor and manual thrombectomy use, which both increased significantly, and drug-eluting stent use which dropped by over 20%. Comparison of mortality rates with median yearly DTB times revealed a correlation between mortality and wait time over the study period. Evaluation of individual DTB times and mortality events, however, revealed shorter patient-specific DTB times were associated with reduced in-hospital mortality and 6-month mortality.
More from this author: Deep brain stimulation linked to declining brain function in Parkinson’s patients, Donor and recipient regulatory T-cells may promote transplant tolerance in mice, Growth factor embedded film promotes robust bone repair, The 3C Study: Alemtuzumab may reduce acute rejection following kidney transplant, Paclitaxel-coated balloons may decrease bronchial stenosis in lung transplants
Image: CC/Patrick J. Lynch
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.



![Vaccines for predicted influenza strains may provide wide protection [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2014/11/18156_lores-75x75.jpg)

