Image-guided assessment of coronary inflammation improves cardiac risk prediction for patients without obstructive coronary artery disease
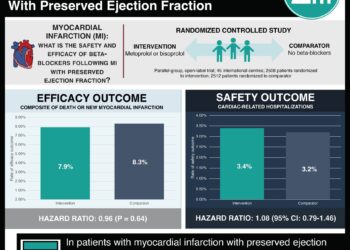
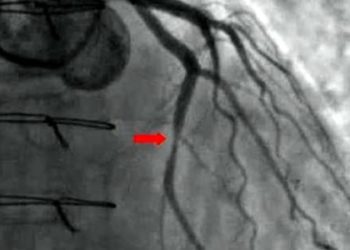
1. Individuals with elevated fat attenuation index scores without obstructive coronary artery disease had significantly increased rates of major adverse ...