Beta-blockers do not lower mortality after myocardial infarction with preserved ejection fraction
1. In this randomized controlled trial, long-term beta-blockers did not impact all-cause mortality among patients with preserved left ventricular ejection fraction (LVEF) following an acute myocardial infarction (MI) and early angiography.
2. Long-term beta-blocker therapy was not associated with a higher risk of adverse events compared to no beta-blocker.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Beta-blockers are a mainstay therapy for heart failure with reduced LVEF. Although historical evidence generally suggested the mortality benefits of beta-blockers following an MI, this predated the diagnostic and therapeutic advancements available today. Furthermore, evidence for beta-blocker therapy specifically for patients with preserved LVEF following acute MIs, especially with early revascularization, is lacking. This trial investigated the effects of long-term beta-blocker therapy against no beta-blocker in patients with an acute MI following coronary angiography who had LVEF ≥50%. At 3.5 years median follow-up, beta-blocker treatment was shown to not impact the risks of death from any cause, new MI, or hospitalization for atrial fibrillation or heart failure, compared to no beta-blocker. Beta-blocker therapy was also not associated with an increased risk of adverse events, including hospitalizations for bradycardia, stroke, or asthma. The study was limited by a lack of blinding and potential for crossover intrinsic to its open-label, pragmatic design. Nevertheless, these findings provided generalizable evidence that beta-blockers did not reduce the composite risk of all-cause mortality or new MI among patients with preserved ejection fraction following an acute MI.
Click here to read the study in NEJM
In-Depth [randomized controlled trial]: This was a randomized, open-label, pragmatic trial to evaluate the impact of long-term beta-blocker therapy initiated early in patients with preserved LVEF. Adult patients were eligible for inclusion at one to seven days after an acute MI if they had undergone coronary angiography demonstrating obstructive coronary disease and had a preserved LVEF (≥50%) demonstrated on echocardiogram. Exclusion criteria included any indication for or contraindication to beta-blocker therapy. From 2017 to 2023, 5020 patients were enrolled and randomized 1:1 to start beta-blocker therapy (either metoprolol targeting 100mg daily or bisoprolol targeting 5mg daily) during their hospitalization or receive no beta-blockers. Patients in the no-beta-blocker group were discouraged from using beta-blockers if there were no other indications than secondary MI prevention. The primary outcome was a composite of death from any cause and a new MI. With the median follow-up of 3.5 years, the composite primary outcome occurred in 7.9% of the beta-blocker group and 8.3% of the no-beta-blocker group (hazard ratio [HR], 0.96; 95% Confidence Interval [CI], 0.79 to 1.16; p=0.64). Correspondingly, the rates of secondary outcomes were similar between the beta-blocker and the no-beta-blocker groups, respectively: death from any cause (3.9% vs. 4.1%; HR, 0.94; 95% CI, 0.71 to 1.24), death from cardiovascular causes (1.5% vs. 1.3%; HR, 1.15; 95% CI, 0.72-1.84), MI (4.5% vs. 4.7%; HR, 0.96; 95% CI, 0.74 to 1.24), hospitalization for atrial fibrillation (1.1% vs. 1.4%; HR, 0.79; 95% CI, 0.48 to 1.31), and hospitalization for heart failure (0.5% vs. 0.9%; HR, 0.91; 95% CI, 0.50 to 1.66). Overall, among patients who had a preserved LVEF following an acute MI, beta-blockers did not impact the composite risk of death from any cause or new MI.
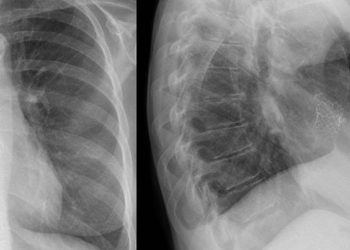
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.