Sofosbuvir therapy may be cost-effective for certain hepatitis C patients
1. From a computer simulation, sofosbuvir-based regimens may be more cost-effective in patients with cirrhosis or previously treated with interferon.
Evidence Rating Level: 2 (Good)
Study Rundown: In 2013, the U.S. Food and Drug Administration (FDA) approved sofosbuvir, a nucleotide analog that inhibits viral RNA synthesis in combination with ribavirin for the treatment of hepatitis C virus (HCV) genotypes 2 and 3. This novel drug can effectively induce a sustained virologic response (SVR) and has fewer side effects than pegylated interferon, which is the current standard of treatment. Sofosbuvir’s main drawback is its price; a four-week regimen currently costs about $28,000 in the U.S. This study used a Monte Carlo simulation and sensitivity analyses to determine the cost-effectiveness of sofosbuvir-based strategies for patients with HCV genotype 2 or 3. From this, it was determined that sofosbuvir-based therapy was cost-effective in patients with cirrhosis and in patients who had previously undergone interferon-based therapy. Conversely, sofosbuvir remains less cost-effective than interferon in non-cirrhotic, treatment-naïve patients. The study’s biggest limitation is that most HCV patients in the U.S. are infected with viral genotype 1 rather than 2 or 3, thereby narrowing its general application. Overall, this study suggests that the high cost of sofosbuvir may restrict its availability to many HCV patients infected with viral genotype 2 or 3.
Click to read the study, published today in the Annals of Internal Medicine
Relevant Reading: Sofosbuvir and ribavirin in HCV genotypes 2 and 3
In-Depth [simulation]: This study employed a Monte Carlo simulation to determine the cost-effectiveness of different treatment strategies for HCV genotype 2 or 3 infection. Patient data from published clinical trials and observational cohorts were used as part of this study. Patient types were defined by HCV genotype, treatment history, and cirrhosis status. Treatment strategies included pegylated interferon plus ribavirin, sofosbuvir plus ribavirin, and pegylated interferon, ribavirin and sofosbuvir. The simulation predicted clinical outcomes (represented by quality-adjusted life-years or QALYs) and costs (represented by the incremental cost-effectiveness ratio or ICER) for each patient type and treatment strategy. The results demonstrated that the pegylated interferon-ribavirin strategy was more cost-effective than sofosbuvir-ribavirin in non-cirrhotic HCV genotype 2 and 3 patients with no prior HCV treatment. In non-cirrhotic patients who had previously been treated with interferon, 12 weeks of sofosbuvir-ribavirin and 12 weeks of interferon-ribavirin-sofosbuvir were the most cost-effective strategies for genotype 2 and 3 patients, respectively. For cirrhotic patients, sofosbuvir-ribavirin was the most cost-effective strategy for genotype 2 and interferon-ribavirin-sofosbuvir was the most cost-effective strategy for genotype 3.
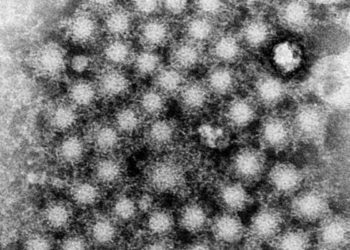
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.