Solanezumab does not improve cognition or functioning in Alzheimer’s disease [EXPEDITION Trials]
Image: PD
1. Solanezumab did not improve cognition or functional ability in mild-to-moderate Alzheimer’s disease at week 80.
2. Solanezumab showed evidence of binding soluble amyloid as measured by plasma and CSF amyloid-beta levels.
Evidence Rating Level: 1 (Excellent)
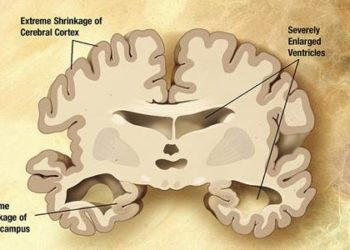
Study Rundown: Two phase 3 clinical trials (EXPEDITION 1 and EXPEDITION 2) examined the ability of solanezumab, a humanized monoclonal antibody against amyloid-beta (Ab), to impact cognition and functional impairment in patients with mild-to-moderate Alzheimer’s disease. In preclinical studies, solanezumab was found to bind preferentially to soluble Ab; this was hypothesized to promote clearance from the brain by shifting the equilibrium toward the soluble form of Ab, thereby reducing plaque formation. However, in the present studies, solanezumab failed to significantly improve cognitive or functional performance at week 80 as measured by the 11- or 14-item cognitive subscales of the Alzheimer’s Disease Assessment Scale (ADAS-cog11 and ADAS-cog14) and the Alzheimer’s Disease Cooperative Study-Activities of Daily Living (ADCS-ADL) scale, among other measures.
Although these results are disappointing, some data suggest that solanezumab may have efficacy in patients with mild Alzheimer’s disease. For example, among those with mild disease, there was a trend toward improvement in ADAS-cog11 score at week 80 and a significant improvement in ADAS-cog14 at week 64, although this was not the primary endpoint. Future investigations of solanezumab may show efficacy in mild Alzheimer’s disease or in asymptomatic individuals with evidence of brain amyloid accumulation. The EXPEDITION 1 and EXPEDITION 2 trials are also valuable in that solanezumab was found to be safe and was not associated with imaging abnormalities; prior studies have raised concern that anti-amyloid therapies might cause amyloid-related imaging abnormalities with edema or hemorrhage. As a class, anti-amyloid treatments warrant further study.
Click to read the study, published today in NEJM
Click to read an accompanying editorial in NEJM
Relevant Reading: Peripheral anti-Aβ antibody alters CNS and plasma Aβ clearance and decreases brain Aβ burden in a mouse model of Alzheimer’s disease
In-Depth [randomized controlled trial]: In EXPEDITION 1 and EXPEDITION 2, two phase 3 clinical trials, 2052 patients with mild-to-moderate Alzheimer’s disease were randomly assigned to receive either solanezumab (400mg) or placebo intravenously, once every 4 weeks for 18 months. Concomitant therapy with cholinesterase inhibitors and/or memantine was allowed. Efficacy measures included both cognitive (ADAS-cog11 and ADAS-cog14; higher scores indicate worse impairment) and functional (ADCS-ADL scale; higher scores indicate improved function) measures. The primary outcomes were changes in scores from baseline to week 80. Additionally, plasma and CSF levels of Ab were measured in a subset of patients.
In EXPEDITION 1, the mean difference between groups (solanezumab minus placebo) in change from baseline to week 80 was -0.8 points for ADAS-cog11 score (p=0.24) and -0.4 points for ADCS-ADL score (p=0.64). In EXPEDITION 2, the mean difference between groups (solanezumab minus placebo) at week 80 was -1.3 points for ADAS-cog11 score (p = 0.06) and 1.6 points for the ADCS-ADL score (p=0.08). A significant difference favoring solanezumab was seen at week 64 but no significant difference was observed at the study end point (week 80). In a subgroup analysis of patients with mild Alzheimer’s disease, a trend toward improvement in ADAS-cog14 score at week 80 was seen in the solanezumab group (between-group difference in change from baseline, -1.7; p=0.06). Among patients with moderate disease, there were no significant differences in ADAS-cog14 score between the solanezumab and placebo groups. Solanezumab significantly increased plasma levels of Ab40 (p<0.001) and significantly decreased CSF levels of free Ab40 (p=0.01). No significant changes were observed in the placebo group.
By Hayley Walker and Adrienne Cheung
More from this author: Low brown fat may explain increased susceptibility to type 2 diabetes in south Asians, Dual PDE3/PDE4 inhibitor may be effective treatment for asthma and COPD, Alefacept may be effective therapy in newly diagnosed type 1 diabetics, Key patient characteristics predict outcomes in children with cardiomyopathy, Remote ischemic preconditioning reduced myocardial injury in CABG patients
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.