2 Minute Medicine Rewind April 11, 2016
Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest
Anti-arrhythmic drugs are commonly used in out-of-hospital cardiac arrest for shock-refractory ventricular fibrillation. Previous studies have shown that patients who receive amiodarone are more likely to achieve a return of spontaneous circulation compared to those who are administered placebo or lidocaine. However, the effects of amiodarone on survival to hospital discharge and neurologic outcomes are unclear. In this randomized controlled trial, 3026 patients with non-traumatic out-of-hospital cardiac arrest and shock-refractory ventricular fibrillation or pulseless ventricular tachycardia were randomized equally to receive amiodarone, lidocaine or placebo to study the effects of these interventions on survival to discharge and neurologic outcomes. Researchers found that there were no significant differences in the percentage of patients that survived to discharge when comparing amiodarone vs. placebo (difference 3.2%, 95% CI -0.4% to 7.0%, p = 0.08), lidocaine vs. placebo (difference 2.6%, 95% CI -1.0% to 6.3%, p = 0.16), or amiodarone vs. lidocaine (difference 0.7%, 95% CI -3.2% to 4.7%, p = 0.70). Using a modified Rankin score to assess neurologic outcomes, the authors also found no significant differences between the interventions. Interestingly, patients that received lidocaine were more likely to achieve a return of spontaneous circulation at emergency department arrival when compared to placebo (difference 5.4%, 95% CI 1.2% to 9.5%, p = 0.01), however a significant effect was not observed in the amiodarone group (difference 1.4%, 95% CI -2.8% to 5.5%, p = 0.52). This study therefore shows that in patients with out-of-hospital cardiac arrest with initial shock-refractory ventricular fibrillation, neither amiodarone nor lidocaine achieve significantly greater rates of survival or neurologic outcomes compared to placebo.
The early postoperative period following abdominal surgery is associated with diaphragmatic dysfunction and a decrease in lung vital capacity. In the event of acute respiratory failure, tracheal reintubation and invasive mechanical ventilation is performed. However, tracheal reintubation is associated with higher mortality, increased healthcare utilization and a longer duration of both intensive care unit (ICU) and hospital stay. Increased mortality has been attributed to complications during the reintubation period, including healthcare-associated infections such as pneumonia. Noninvasive ventilation (NIV) has proven effective in nonsurgical cases of acute exacerbation of chronic obstructive pulmonary disease and cardiogenic pulmonary edema. At this time, however, there is no evidence to support the use of NIV in surgical patients with hypoxemic acute respiratory failure after abdominal surgery. In this randomized controlled trial, 293 patients that had undergone abdominal surgery and developed hypoxemic respiratory failure were randomized to receive either standard oxygen therapy or NIV delivered via facial mask to evaluate whether the application of NIV can prevent reintubation and invasive mechanical ventilation. Researchers found that within 7 days of randomization, patients in the NIV were less likely to require reintubation compared to patients in the standard oxygen therapy group (difference -12.4%, 95% CI -23.5% to 1.3%, p = 0.03). Patients in the NIV group were also less likely to develop pneumonia after 7 days (difference -11.93%, 95% CI -20.94% to -2.93%, p=0.005) and 30 days of follow-up (difference -15.09%, 95% CI -25.72% to -4.45%, p=0.003). There were no significant differences between the groups with respect to 30- or 90-day mortality. This study therefore shows that in patients with hypoxemic respiratory failure following abdominal surgery, NIV may be used in reducing rates of tracheal reintubation and related complications.
Approximately half of HIV-positive individuals in sub-Saharan Africa are unaware of their serostatus. While wider availability of facility-based HIV testing and counseling services and community-based HIV testing and counseling strategies have helped to increased testing coverage, achieving high levels of testing coverage remains a challenge in many countries. Men, in particular, are less likely to undergo testing compared to women. HIV self-testing is a promising approach with the potential to increase access to testing for individuals and/or couples in a way that is both confidential and empowering. Little is known on how HIV self-testing can be best distributed in hard-to-reach or high-risk individuals. One such strategy is secondary distribution, whereby an individual who is given multiple tests can distribute them to sexual partners or others in their social network. In this cohort study, the effects of secondary distribution of self-tests by 265 HIV-negative women were assessed. Outcomes included the number of self-tests distributed by participants, the proportion of participants whose sexual partners used a self-test, couples testing and sexual behaviour after testing. Women seeking antenatal care or post-partum care were recruited, as there is a high risk of HIV transmission in these populations. Female sex workers were also recruited. Researchers found that nearly all participants with a primary sexual partner at baseline distributed a self-test to that partner: 91% in the antenatal care group, 86% in the post-partum care group, and 75% of female sex workers. Female sex workers were also very likely to distribute self-tests to other sexual partners, with over 80% of participants distributing one or more self-tests to commercial sex clients. Furthermore, participants distributed self-tests to individuals that were not sexual partners, where roughly 75% of the women from the antenatal or post-partum care group, and 32% of female sex workers distributed one or more self-tests to a female friend. Of the 445 self-tests distributed to male sexual partners, 442 (99%) were reported as having been used, almost always in the presence of the study participant. The proportion of males with an HIV-positive result ranged from 2% in the post-partum care group, to 14% in the female sex worker group. According to the study participants, sexual intercourse was less likely after their sexual partners tested HIV-positive (p<0.0001), and condom use increased after a positive result (p=0.0018). This study therefore shows that the provision of multiple HIV self-tests to women at high risk of HIV infection can be an effective means of promoting HIV testing among their sexual partners and facilitating safer sexual decisions.
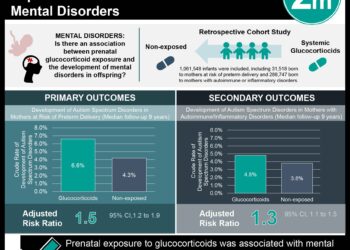
Antenatal betamethasone for women at risk for late preterm delivery
Infants born at 34-36 weeks gestation or late preterm are at an increased risk of experiencing adverse respiratory outcomes compared to those born at 37 weeks or later. Antenatal glucocorticoids are widely used in obstetrics for pregnancies at risk of early preterm delivery in women likely to deliver before 34 weeks gestation. Currently, there is a lack of evidence to support the administration of antenatal glucocorticoids in women at risk of preterm delivery after 34 weeks. In this randomized controlled trial, 2827 women likely to deliver in the late preterm period were randomized to receive betamethasone or placebo to determine whether antenatal glucocorticoids may decrease the incidence of respiratory and other neonatal complications in this group. The primary outcome of this study was a composite end point describing the need for respiratory support within 72 hours after birth, consisting of one or more of the following: the use of continuous positive airway pressure (CPAP), high-flow nasal cannula for at least 2 consecutive hours, supplemental oxygen with a fraction of inspired oxygen of at least 0.30 for at least 4 continuous hours, extra-corporeal membrane oxygenation (ECMO) or mechanical ventilation. Researchers found that the rate of the primary outcome was significantly less in the betamethasone group compared to placebo (RR 0.80, 95% CI 0.66 to 0.97, p = 0.02). This meant that in order to prevent one case of the primary outcome, 35 women would need to be treated with betamethasone (NNT 35, 95% CI 19 to 259). The rate of severe respiratory complications was also significantly less in the intervention group compared to placebo (RR 0.67, 95% CI 0.53 to 0.84, p < 0.001). For severe respiratory complications, the number needed to treat to prevent one case was 25 (NNT 25, 95% CI 16 to 56). Infants from the betamethasone group were also less likely to spend 3 or more days in the intensive or intermediate care nursery (p = 0.03) and had a shorter time until first feeding (p = 0.004). Infants from the intervention group, however, had a higher incidence of neonatal hypoglycemia (RR 1.60, 95% CI 1.37 to 1.87, p<0.001). This study therefore shows that the administration of betamethasone to women at risk for late preterm delivery may significantly reduce the rate of neonatal respiratory complications.
Out-of-hospital cardiac arrest in high-rise buildings: delays to patient care and effect on survival
The increasing number of people living in high-rise buildings presents new challenges in the delivery of emergency health services. In the event of cardiac arrest, rapid defibrillation and high-quality cardiopulmonary resuscitation (CPR) are essential for survival, with an absolute decrease in survival of 7-10% for every 1-minute delay to defibrillation. In this retrospective cohort study, data from the Toronto Regional RescuNet Epistry database was used to compare the rate of survival to hospital discharge after out-of-hospital cardiac arrest at different vertical heights in residential buildings, specifically higher floors versus lower floors (<3 floors). The final study population comprised of 7842 patients. Researchers found that there was a greater delay from the time or arrival of 911-initiated first responders on scene to patient contact on the higher floors (p = 0.01). With respect to survival, 4.2% of patients living on lower floors survived, compared to 2.6% of patients living on higher floors (p = 0.002). This correlation persisted in a multivariable regression analysis, where cardiac arrest on higher floors was found to be independently associated with decreased survival to hospital discharge (OR 0.70, 95% CI 0.50 to 0.99). This study therefore shows that in high-rise buildings, the survival rate after out-of-hospital cardiac arrest is lower in patients residing on higher floors.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.